Even if you control your diabetes with insulin shots, you are probably already accustomed to shunning sugar and cutting carbs. But what about alcohol? Is it safe to enjoy wine, beer, or liquor while using insulin to manage your type 1 or type 2 diabetes?
Alcohol and diabetes can mix…sometimes
“There are numerous factors (that) determine the safety of drinking alcohol while taking insulin,” says Kristen Smith, MS, RD, a spokesperson for the Academy of Nutrition and Dietetics. “It is best to discuss drinking alcohol with your healthcare provider for an individualized approach.”
Some of these factors include overall health status and whether you are adept at managing your blood sugar, says Smith. For example, patients who are also dealing with high blood pressure and/or high cholesterol in conjunction with diabetes might be told to think twice about having that drink. Same for anyone with a diagnosis of diabetic neuropathy or with a history of pancreatitis. If your diabetes is under control and you don’t have any other related conditions, however, it is possible that your doctor will give you the green light to enjoy alcohol in moderation (which according to the U.S. Department of Health and Human Services is up to one drink a day for women and two drinks a day for men).
“A glass or two of wine with dinner every now and then will not at all derail an individual’s efforts to manage their diabetes, but multiple [drinks] every night becomes another story,” says Tom Kalista, Pharm.D., a consultant pharmacist with the National Community Pharmacists Association.
Alcohol, diabetes, and hypoglycemia
If you have diabetes and choose to drink, you need to be very aware of how alcohol can affect you, says Jeff Fortner, Pharm.D., an associate professor at Pacific University’s School of Pharmacy in Forest Grove, Oregon, and a member of the SingleCare Medical Review Board.
Alcohol lowers blood sugar.
“A potential but little-known effect of drinking more than moderate amounts of alcohol is [that] it causes blood sugar levels to drop for a period of a couple of hours to even a whole day,” Dr. Fortner says.
This applies to everyone, but it is especially significant for people with diabetes since keeping blood sugar in check is key to overall management of their condition, adds Dr. Kalista. “It is very important to be aware of where their blood sugar is before [drinking] and where it will likely go as a result, without forgetting to account for food, other drinks, or medication that will also affect blood sugar,” he says.
And what about the insulin itself? Will it trigger a drug-drug interaction? Probably not.
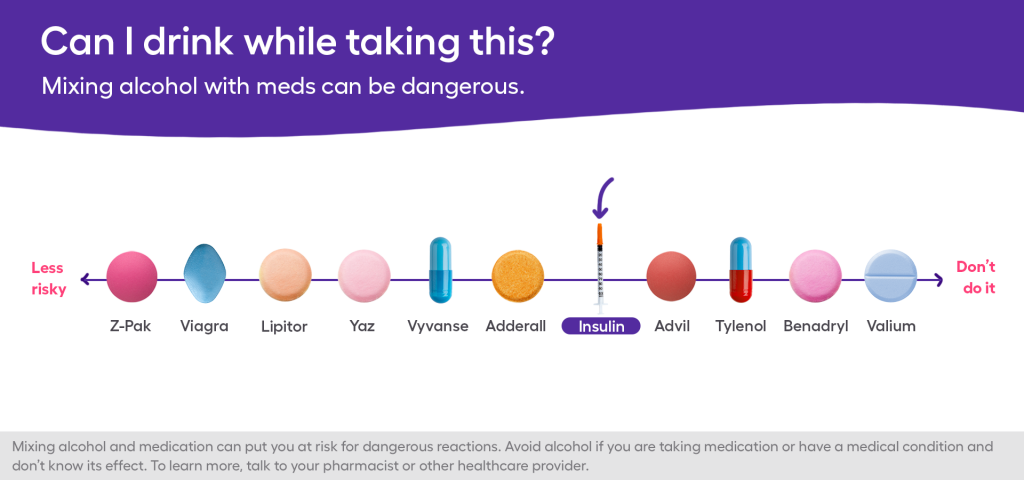
Unlike some medications (such as benzodiazepines, which are dangerous to consume alongside alcohol under any circumstances), insulin and alcohol “do not interact directly,” says Dr. Kalista. With insulin, the concern is more about how your body handles the blood sugar roller coaster associated with both alcohol and diabetes. In other words, it is important to recognize that drinking alcohol can trigger a hypoglycemic episode. People with diabetes are already at risk of hypoglycemia simply because of the nature of the condition. With alcohol in the mix, the risk becomes even greater—and it also makes the treatment of diabetes much more complicated, Dr. Kalista says.
Intoxication mimics hypoglycemia.
Furthermore, the symptoms of hypoglycemia—confusion, dizziness, irritability, headache and fatigue—are very similar to the symptoms of intoxication, Smith and Dr. Fortner say. This can spell trouble.
“A major concern of drinking too much [for people with diabetes] is that alcohol intoxication may hide the symptoms of severely low blood sugar, which can lead to life-threatening conditions,” Dr. Fortner says.
Basically, this means that you might not realize you need insulin because you think you are just, well, inebriated. Likewise, using insulin while your blood sugar is too low is also problematic because your blood sugar will just continue to drop. Next thing you know, you are in an ambulance or the emergency room (Smith emphasizes the importance of seeking medical attention for signs of severe hyperglycemia, whether the situation involves alcohol or not).
Alcohol impairs your liver.
To add insult to injury, if you are overdoing it on the alcohol, your liver is going to be too busy dealing with that to concern itself with your blood sugar, which will only add to your body’s confusion over what is happening.
“Our liver prioritizes getting rid of toxins before it spends energy to convert glycogen back into glucose, so as long as there is alcohol to metabolize, the liver isn’t doing as much to regulate blood sugar levels, so blood sugar drops until the alcohol is out of the blood,” Dr. Fortner explains.
Safety guidelines for combining alcohol and diabetes
If you have type 1 or type 2 diabetes and your doctor decides that drinking in moderation is okay for you, Dr. Fortner and Smith recommend sticking to the following guidelines in order to keep yourself safe:
- Never drink on an empty stomach. In fact, it is best to eat while consuming alcohol because food slows the absorption of alcohol and raises blood sugar levels.
- Test your blood sugar before drinking to make sure it isn’t already low. If it is, get it into the safe zone before imbibing.
- Avoid sugary mixers, sweet wines, or liquor mixed with sweetened soda or juice. Instead, go for liquor mixed with club soda or water (a diet soft drink would be okay, too), dry wine, or low-carb beer.
- Take small sips and drink slowly. Ideally, alternate sips of your drink with sips of water.
- Wear a medical alert ID that states you have diabetes in case you have a hypoglycemic episode.
- Inform the people you are with that you have diabetes for the same reason, so they can get help if needed.











