Whether they don’t like the taste of liquid, are afraid of or unable to swallow pills successfully, or fear injections, some children struggle to successfully take their medications.
For parents of children diagnosed with autism spectrum disorder (ASD), making sure they’re taking medication that keeps them healthy can be an especially difficult task. This guide will explain why children with autism reject medication and specific tips to make taking medicine as easy as possible.
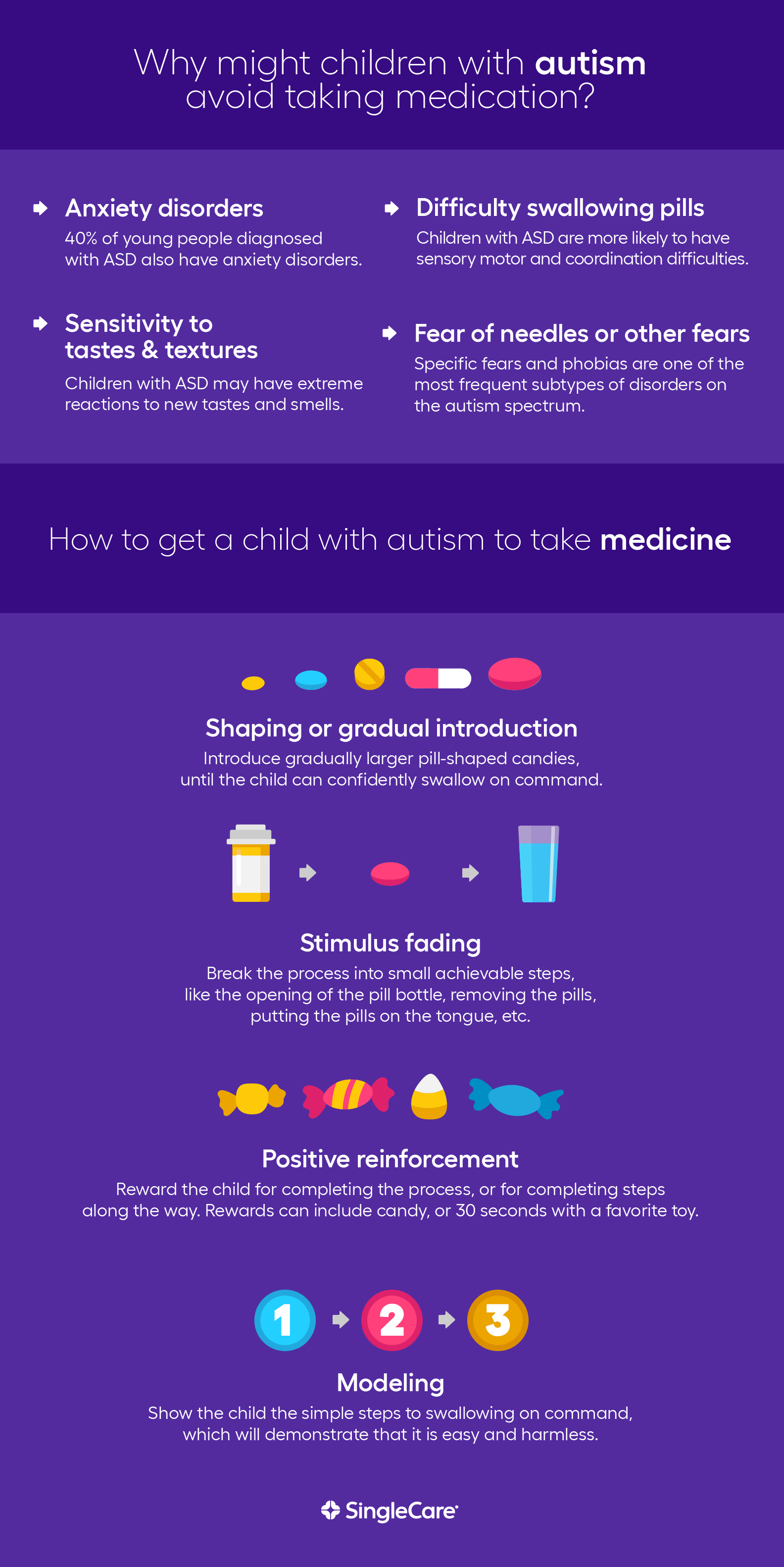
Why do some children with autism avoid taking medication?
Medication refusal can happen on any day for any reason, but if your child consistently refuses medication, it can be helpful to understand why. It’s important to avoid blaming the child and work with them to overcome their concern.
Autism and anxiety disorders
“Forty percent of young people diagnosed with autism spectrum disorder have clinically elevated levels of anxiety or at least one anxiety disorder, including obsessive-compulsive disorder,” according to the Anxiety and Depression Association of America,
Anxiety disorders like these may be a reason for taking medication, and can also be a reason why your child refuses medication. Taking medication may also represent a change in routine—a common trigger of distress among children diagnosed with ASD.
Sensitivity to tastes and textures
Studies have shown that food selectivity, aka “picky eating,” is more common among children with autism than the general population. Food selectivity may be linked to heightened sensitivity to tastes and smells.
Children with autism may experience the world around them differently. A sound, sight, or taste that seems unremarkable to most people can trigger extreme reactions. In other words, liquid medicine that smells fine to you could smell disgusting to a child with autism.
Difficulty swallowing pills
Swallowing is a complex process requiring coordinated movements by the tongue, hard palate, and esophagus. Because children diagnosed with ASD are more likely to have sensory-motor and coordination difficulties, some simply aren’t able to activate the motor functions needed to swallow on command.
During the oral phase of swallowing, the tongue and hard palate must propel the food toward the back of the throat. Once this happens, the swallow reflex should activate. If it doesn’t, the child may cough, choke, spit-up, or get the pill stuck in their throat.
Fear of needles or other fears
Specific fears and phobias are some of the most frequent subtypes of disorders for ASD. Children with autism are prone to common childhood fears (like fear of needles), but uncommon fears may cause anxiety as well. A 2013 study found that 41% of children with autism had unusual fears. Some unusual fears reported by parents of children with autism include vacuum cleaners, toilets, and elevators.
So, a child with autism may fear negative side effects of the medication or the side effects of the medication may be associated with another trigger. Fear of the toilet is one of the more common “uncommon” fears, so a medication with digestive side effects could exacerbate that fear.
How to teach a child with autism to take medicine
The time must be right to teach any child to take medicine.
The skill of pill swallowing is the most important for a child to learn. Many medications are only available in pill form or are much less expensive in pill form. Whether your child requires long-term treatment with medication, or simply needs antibiotic treatment to overcome an infection, being able to swallow pills will improve their prognosis and overall health.
According to pillswallowing.org, a service of New York’s Northwell Health: “If your child can follow instructions and is able to manage swallowing ‘chunky,’ textured foods (e.g., oatmeal or chunky applesauce) without gagging or choking and swallows mouthfuls of liquid without it spilling from her mouth or causing coughing/gagging, she should be ready to learn pill swallowing.”
Around age 6 or 7, most children have the motor skills, attention span, and ability to follow instructions required to successfully swallow pills. For children with autism, these abilities may take longer to develop. You may want to ask a medical professional for an assessment of whether your child is ready or not.
Once you’ve decided to teach your child to take pills, here are some techniques to use.
Shaping or gradual introduction
One standard pill swallowing instructional technique that is used for all children is called shaping, or the gradual introduction of new behaviors in small steps.
Shaping is a term used in behavior modification therapy. Basic concept: You find the easiest possible introduction to a difficult task, and then increase the difficulty as the person has success. The successful completion of each task is rewarded with positive reinforcement.
For pill swallowing, the process is simple. You start by giving the child water to practice swallowing on command. Then, you begin introducing small candy “pills” to swallow such as cake decorations. Increase the size of the “pills” until the child is a pill swallowing expert. This candy-shaping chart shows the types of “pills” you can use.
For liquid medicine, you can start by introducing small amounts of a liquid your child is already familiar with like water or juice. Once up to the required dosage, mix in or switch to the prescribed medication.
Stimulus fading
Stimulus fading is a behavior modification and teaching tool with all types of applications. For example, stimulus fading flashcards can be used to teach vocabulary. The initial flashcard might show a picture of a cat, along with the word cat. In the next flashcards, the image of the cat would slightly fade until it is gone altogether and only the word remains.
The technique was also used in the case of a 3-year-old child with autism who refused to take liquid medicine. The boy would yell or run away when presented with liquid medicine, and refused to drink milk or juice with medicine mixed in.
At first, clinicians simply presented the boy with an empty syringe. Then they required him to open his mouth with the empty syringe present. The next steps involved slowly decreasing the distance between the boy and the empty syringe until the syringe was less than an inch from his mouth. Next, the boy was required to ingest water at increasing volumes, and then, once that was completed, the boy was given a placebo liquid medication. The final step was for the clinician to leave the room while the boy’s mother took over the process.
The technique requires dedication but can be successful. By the end of the stimulus fading process, clinicians reported the boy “often smiled and requested the medicine during the last dozen or so sessions of treatment.”
Positive reinforcement
Experts report that simply maintaining a positive attitude can help children take medicine without fear or resistance. But positive reinforcement in the form of rewards can also help.
Positive reinforcement can be combined with other techniques. In the case of the stimulus fading treatment above, positive reinforcement was a key aspect of the program. When the boy successfully completed a step, the clinician gave him one or two pieces of candy or 30 seconds of access to a toy.
Modeling
Modeling is showing a child that the action you want them to take is easy and harmless. When a child sees a parent successfully complete the action of pill swallowing or taking liquid medicine from a syringe, they may feel less anxiety about doing it themselves.
Modeling can be a more successful technique for children with autism who may struggle to understand spoken instructions. Seeing a person perform a task, and then being given the chance to imitate the task, may be a more effective way to learn.
Keep pill-like objects or placebos on hand to model proper medicine-taking behavior for your child with autism.
Special steps with liquid medication
In addition to using the steps above to introduce liquid medication to a child with autism, you may also be able to introduce additives to make the medication taste better.
Ask your pharmacist if it’s okay to mix the liquid medication with water, juice, or another liquid that will hide the medication’s taste. Your pharmacist will be able to make sure certain drinks or foods don’t interact with the medication. You should also only use a small amount of additional liquid because you need to be sure that the child is ingesting enough of the medication.
If your child refuses liquid medication, you can ask a medical professional if the same medication is available in a chewable tablet form.
Special steps with pills
Ideally, the techniques above will allow your child to become a pill swallowing expert. If not, there are a few strategies you can try.
One is to have the child swallow a favorite liquid along with the pill. PillSwallowing.org recommends these three strategies.
- Two-gulp method: Place the pill on the tongue. Take one gulp of liquid and swallow it without swallowing the pill. Then, take a second gulp of liquid right away, swallowing the pill and the water together.
- Straw technique: Place the pill far back on the tongue. Then have your child drink the liquid through a straw, quickly. If the child is focused on swallowing their favorite liquid, rather than thinking about the pill, the pill will likely go down their throat. [Straw Technique Video]
- Pop bottle method: Place the pill anywhere in the mouth. Have the child seal their lips and mouth over an open drink bottle, and maintain contact between the bottle and lips while taking a big gulp of the drink. This should allow the child to easily swallow both the liquid and the pill. [Pop Bottle Method Video]
Another technique is to use food as a method of concealing the pill. Some children who struggle to swallow pills have no problem gulping them down as part of a spoonful of yogurt, applesauce, or peanut butter.
Dealing with fear of needles
An extreme fear of needles is associated with autism in children. A child’s inability to have blood taken or receive injections can, in some cases, be life-threatening. So children with an extreme fear of needles must sometimes be sedated or restrained.
A better solution is to work to overcome fear of needles.
In the case of a boy who required regular blood monitoring for diabetes, a stimulus fading method was used. The needle was positioned increasingly closer to the boy’s finger over a period of training sessions until he was able to successfully complete blood draws.
Another approach, used in conjunction with stimulus fading, is to try to understand the nature of a child’s needle anxiety, or what causes them to fidget during medical procedures.
Karen Levine, Ph.D., writing for Autism Spectrum Monthly, suggests three steps for addressing fear of needles in children with autism.
- Step 1: Figure out the components of the event the child fears.
- Step 2: Determine and use self- or co-regulation strategies (such as letting the child listen to their favorite music or play with toys).
- Step 3: Determine the techniques to use for gradually exposing the child to the components from Step 1, and then pair these with the anxiety-decreasing measures from Step 2.
In the case of one 10-year-old boy with autism (who had a long-standing fear of needles), his family identified that many of the elements of visiting a medical office created fear for their child. They created a play medical office with Legos and allowed the boy to desensitize himself to the situation by engaging in medical office play. By the end of the treatment, the boy was able to complete a blood draw, and “he was so proud of himself that he even asked to do it again!”
The rewards of successful medication-taking go beyond physical health
In the case of the 10-year-old with an extreme fear of needles, being part of the process to eliminate the fear didn’t just make him safer, it actually made him proud.
Parents of children with autism can view the process of overcoming fear and anxiety associated with medication as an opportunity as well as a challenge. Helping your child overcome this fear can improve their self-image, and teach them to confront other anxiety-inducing situations in their daily life.
Here are some resources for further reading on the topic.
- PillSwallowing.com: An Educational Website to Improve Pill Swallowing Skills
- Establishing Compliance with Liquid Medication Administration in a Child with Autism, Journal of Applied Behavior Analysis
- Stimulus Fading and Differential Reinforcement for the Treatment of Needle Phobia in a Youth with Autism, Journal of Applied Behavior Analysis
- Treating Fears and Phobias in Children with ASD, Autism Spectrum Quarterly











