Key takeaways
The most significant and serious methotrexate interactions are with certain antibiotics, PPIs, and NSAIDs since these are common medications individuals consume.
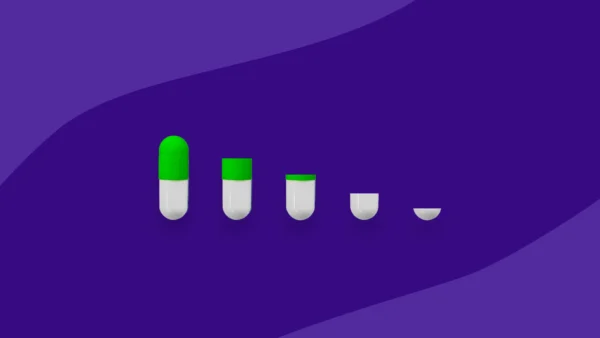
The dose of methotrexate is also an important consideration when evaluating the type and risk of possible drug interactions.
-
- Low-dose methotrexate does not impose too much risk in combination with many medications.
- High doses of methotrexate, common in the management of certain forms of lymphoma and leukemia, when taken in combination with medications that may increase blood levels as well as impact clearance, raise the risk of serious side effects.
-
Adverse effects that can result include increased side effects like mucositis (ulcers throughout the gastrointestinal tract), hepatitis, or, in the worst-case scenarios, bone marrow suppression, renal toxicity resulting in renal impairment, and liver disease.
A complete list of medications should always be offered to a healthcare professional for patients prescribed methotrexate so that a thorough evaluation of possible drug interactions can be conducted.
Drug interactions | Food interactions | Other interactions | Avoiding interactions | When to see a doctor
Methotrexate, known by the brand name Trexall, is recognized within a few pharmacologic categories, given its broad use in many medical conditions. It is known as an antineoplastic (chemotherapy) agent, a disease-modifying antirheumatic drug (DMARD), and an immunosuppressant agent. Methotrexate is available in an oral and injectable formulation, is indicated for the treatment of rheumatoid arthritis, and is a major chemotherapeutic choice for various types of cancer. Methotrexate is also employed in many autoimmune diseases, such as psoriasis, systemic lupus erythematosus (SLE), inflammatory bowel disease (IBD), and others. Methotrexate has distinct mechanisms of action for its use as chemotherapy versus immunosuppression in autoimmune diseases. Certain antibiotics, proton pump inhibitors, non-steroidal anti-inflammatory drugs (NSAIDs), antiepileptics, diuretics, and other medications that can cause kidney problems, like cyclosporine or cisplatin, can result in problems when taken with methotrexate. Given its mechanism of action, methotrexate should also not be administered with folate supplementation. It’s important to be aware of methotrexate interactions as other drugs can impact its effectiveness, potentially leading to toxicity and severe side effects.
Methotrexate drug interactions
Methotrexate can interact with any medication, impacting its free drug concentration in the blood or its elimination. Many serious interactions occur with higher doses of methotrexate employed for its antineoplastic mechanism of action. They can be serious if not identified ahead of time, resulting in permanent renal damage. Many commonly used drug classes cause interactions with methotrexate, including certain, (PPIs), and non-steroidal anti-inflammatory drugs (NSAIDs). Other less commonly prescribed and used drugs and supplements can potentially interact with methotrexate. Therefore, it’s critical to be aware of these possible drug interactions to avoid the development of unnecessary methotrexate toxicity.
Antibiotics
High doses of methotrexate administered with certain antibiotics may increase the serum concentrations of methotrexate. Lower doses of methotrexate, such as those generally implemented for rheumatologic conditions, carry less of a risk than higher doses of methotrexate employed for its antineoplastic effects.
The penicillin and tetracycline drug class specifically carries this risk. In addition to penicillin itself, other interacting penicillin class antibiotics, including amoxicillin, nafcillin, oxacillin, and piperacillin, are known to interact with methotrexate. The mechanism of this interaction is not fully determined, but it is presumed that penicillins compete with methotrexate for excretion sites in renal tubules. This impacts methotrexate elimination and ultimately increases the risk of methotrexate toxicity. The extent of this interaction is presumed to be increased with increased doses of either penicillin antibiotics or methotrexate.
Tetracycline antibiotics, including doxycycline, minocycline, and tetracycline itself, may increase the serum concentrations of methotrexate, but this is likely not a clinical issue when using antirheumatic doses of methotrexate. If used concomitantly, individuals should be monitored for the toxic effects of methotrexate, especially when either a penicillin or tetracycline antibiotic is initiated or the dose increased. In the setting of high-dose methotrexate with antibiotics in either of these drug classes, alternative agents should be used for treatment to avoid any possibility of toxicity.
In addition to these 2 classes of antibiotics, significant drug-drug interactions exist between methotrexate and trimethoprim–sulfamethoxazole. Unlike the interaction between methotrexate and penicillin antibiotics, which is likely to only be clinically significant with higher doses of methotrexate, many case reports describe the development of methotrexate toxicity (including severe bone marrow suppression, at times fatal) in patients taking even low doses of weekly methotrexate for autoimmune conditions with trimethoprim–sulfamethoxazole. Given the significance of this interaction, any individual to be started on methotrexate should avoid concomitantly receiving trimethoprim–sulfamethoxazole. If taken together, contact a healthcare provider immediately to increase monitoring of methotrexate serum levels and signs or symptoms of toxicity. An alternative antibiotic should replace trimethoprim–sulfamethoxazole.
Non-steroidal anti-inflammatory drugs (NSAIDs)
Coadministration of methotrexate with NSAIDs, which include diclofenac, ibuprofen, ketorolac, meloxicam, and naproxen, may increase the blood levels of methotrexate. NSAIDs may decrease renal elimination of methotrexate by inhibiting renal transport proteins or by decreasing blood perfusion of the kidneys. The severity of this interaction is likely greater with higher doses of methotrexate, such that the coadministration of NSAIDs and higher doses of methotrexate should be avoided. Ibuprofen may decrease methotrexate clearance by up to 40%. While the same level of evidence doesn’t exist across the board for NSAIDs, given their similar properties, they are presumed to respond similarly. Caution should still be exercised during the coadministration of NSAIDs and lower doses of methotrexate, even in people who have received methotrexate long-term. Some studies have demonstrated increased methotrexate levels within one day of coadministration, so avoidance is the safest bet.
Proton pump inhibitors
Methotrexate consumed with proton pump inhibitors (PPIs) may also increase the blood concentration of methotrexate. Medications within the class of PPIs include omeprazole and pantoprazole, among others. The mechanism of this interaction isn’t entirely determined but is likely due to inhibition of methotrexate elimination due to PPI inhibition of certain activities within kidneys. In a study including 79 patients, PPI consumption was associated with delayed methotrexate elimination. Pantoprazole prescribing information recommends temporarily holding the PPI therapy for patients receiving high-dose methotrexate due to the interaction, which may result in methotrexate toxicity. The clinical significance of this interaction is highest with antineoplastic doses of methotrexate, but if a patient on antirheumatic doses of methotrexate can receive an alternative class to PPIs, it is the safest option to avoid any risk of methotrexate toxicity and delayed methotrexate elimination.
Anticonvulsants
Anticonvulsants are less commonly prescribed medications than the antibiotics, NSAIDs, and PPIs already described to interact with methotrexate, but may also interact with methotrexate and cause devastating effects.
Levetiracetam may increase the serum concentrations of methotrexate and cause delayed methotrexate elimination, presumably through competing with methotrexate for active tubular excretion in the kidney. Individuals receiving concomitant therapy should be evaluated for increased methotrexate blood concentrations and associated toxicities.
Unlike the result of all the interactions discussed so far, coadministration of methotrexate and phenytoin may increase the serum concentrations of methotrexate but may also decrease the serum concentrations of phenytoin, a dual interaction. The mechanism for these interactions is not fully established and is likely the result of multiple scenarios. Individuals receiving this combination of medications must be closely monitored through therapeutic drug monitoring of both phenytoin and methotrexate serum concentrations. Methotrexate serum concentrations should be monitored more closely while receiving phenytoin and the onset of symptoms associated with methotrexate toxicity.
The interaction between valproic acid and methotrexate is also unique in that the interaction is a possible decrease in the serum concentration of valproic acid, such that doses may need to be increased to avoid the increased frequency of seizures or other symptoms managed by the valproic acid. Methotrexate and valproic acid likely compete for protein binding, leading to valproic acid displacement and increased metabolism.
Probenecid
Probenecid is a uricosuric agent, a drug used to control elevated uric acid levels in patients with gout. Newer drug classes and agents have largely replaced probenecid for this indication. However, given its unique mechanism of action, probenecid is still occasionally used for its ability to serve as a pharmacokinetic enhancer of penicillin in the management of sexually transmitted infections by blocking their route of elimination. Probenecid can also serve as a renal protective agent in patients requiring treatment with an antiviral known as cidofovir. While few people receive probenecid, it can significantly interact with methotrexate, either in high or low doses, by probenecid inhibition of renal tubular secretion of methotrexate, allowing methotrexate to accumulate. Prescribing information for both probenecid and methotrexate mentions the risk of developing severe adverse reactions when these medications are taken concomitantly. If the use of methotrexate is required, then patients should be monitored closely for adverse reactions related to increased methotrexate blood concentrations with a possible methotrexate dose reduction.
Methotrexate food interactions
The use of high-dose methotrexate interacts with cola-containing drinks, with an observed increase in serum concentrations of methotrexate. Cola beverages contain high amounts of inorganic acids, which lower the urinary pH and possibly delay methotrexate elimination. Patients requiring antineoplastic doses of methotrexate should avoid cola-containing drinks during and for several days following methotrexate infusions, ideally until adequate methotrexate elimination is confirmed with routine therapeutic drug monitoring. Licorice may also increase methotrexate blood levels due to delayed methotrexate elimination by inhibiting specific transporters responsible for eliminating methotrexate. Finally, methotrexate may suppress the immune system, so avoiding unwashed fruits and vegetables or unpasteurized milk and soft cheeses is best.
Other methotrexate interactions
Other types of methotrexate interactions to be aware of include those that may enhance the toxicities associated with methotrexate.
Methotrexate and alcohol
Alcohol may enhance the hepatotoxic effects of methotrexate, so alcohol consumption should be limited throughout the course of methotrexate. In patients with autoimmune conditions being evaluated for treatment with methotrexate, it is considered contraindicated in those individuals with alcoholism or alcoholic liver disease.
How to minimize methotrexate interactions
Always carry a complete list of medications, including supplements, on your person. Any time you receive medical advice with new therapy recommendations, provide this list so that a thorough review and drug information assessment can be performed. This can minimize the risk of drug interactions.
When to talk to a healthcare provider about methotrexate interactions
This article is not a complete list of methotrexate interactions. Discuss any new signs or symptoms, no matter how mild, with your healthcare professional when starting a new medication. Be mindful of the risk of additive side effects and direct drug interactions, which may occur when methotrexate is used in combination with prescription and over-the-counter medications or supplements. Communicate directly with a healthcare professional anytime you require methotrexate so that a comprehensive review of interactions with medications, diet, and conditions can occur to ensure a proper monitoring plan is put in place.
Sources
- Methotrexate, StatPearls (2023)
- Pharmacokinetic interaction between high-dose methotrexate and amoxicillin, Therapeutic Drug Monitoring (1993)
- Pharmacokinetic interaction between methotrexate and piperacillin/tazobactam resulting in prolonged toxic concentrations of methotrexate, The Journal of Antimicrobial Chemotherapy (2006)
- Characterization of methotrexate transport and its drug interactions with human organic anion transporters, The Journal of Pharmacology and Experimental Therapeutics (2002)
- High-dose methotrexate-doxycycline interaction, The Annals of Pharmacotherapy (1999)
- Methotrexate and trimethoprim: A fatal interaction, British Journal of Rheumatology (1998)
- Quantitative evaluation of the drug-drug interactions between methotrexate and nonsteroidal anti-inflammatory drugs in the renal uptake process based on the contribution of organic anion transporters and reduced folate carrier, The Journal of Pharmacology and Experimental Therapeutics (2004)
- The effects of a salicylate, ibuprofen, and naproxen on the disposition of methotrexate in patients with rheumatoid arthritis, European Journal of Clinical Pharmacology (1992)
- Concomitant use of low-dose methotrexate and NSAIDs and the risk of serious adverse events among patients with rheumatoid arthritis, Pharmacoepidemiology and Drug Safety (2018)
- Delayed elimination of methotrexate associated with co-administration of proton pump inhibitors, Anticancer Research (2010)
- Protonix IV (pantoprazole) [prescribing information], Philadelphia, PA: Wyeth Pharmaceuticals Inc; September 2012
- Drug-drug interaction between methotrexate and levetiracetam resulting in delayed methotrexate elimination, The Annals of Pharmacotherapy (2014)
- Weekly methotrexate may reduce valproate levels causing relapse of genetic generalized epilepsy, Epilepsy & Behavior Reports (2021)
- Uricosuric drugs: The once and future therapy for hyperuricemia?, Current Opinion in Rheumatology, 2014
- Prolongation and enhancement of serum methotrexate concentrations by probenecid, British Medical Journal (1978).
- Severe pancytopenia in a patient taking low dose methotrexate and probenecid, The Journal of Rheumatology (1991)
- Cola beverage and delayed elimination of methotrexate, British Journal of Clinical Pharmacology (2010)
- A previously unknown drug-drug interaction is suspected in delayed elimination of plasma methotrexate in high-dose methotrexate therapy, The Annals of Pharmacotherapy (2020)
- Methotrexate [prescribing information], Eatontown, NJ: West-Ward Pharmaceuticals Corp; August 2020