Key takeaways
Ozempic is a glucagon-like peptide-1 (GLP-1) agonist medication approved to manage blood sugar levels in adults with Type 2 diabetes.
Ozempic is not for people who have a personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome Type 2, or people who have allergic reactions to it. Other health conditions that may require caution include issues with the pancreas, kidneys, gallbladder, or vision, as well as pregnancy.
The best way to determine if Ozempic is a good option for you is to consult your healthcare provider, who can develop an individualized treatment plan for you.
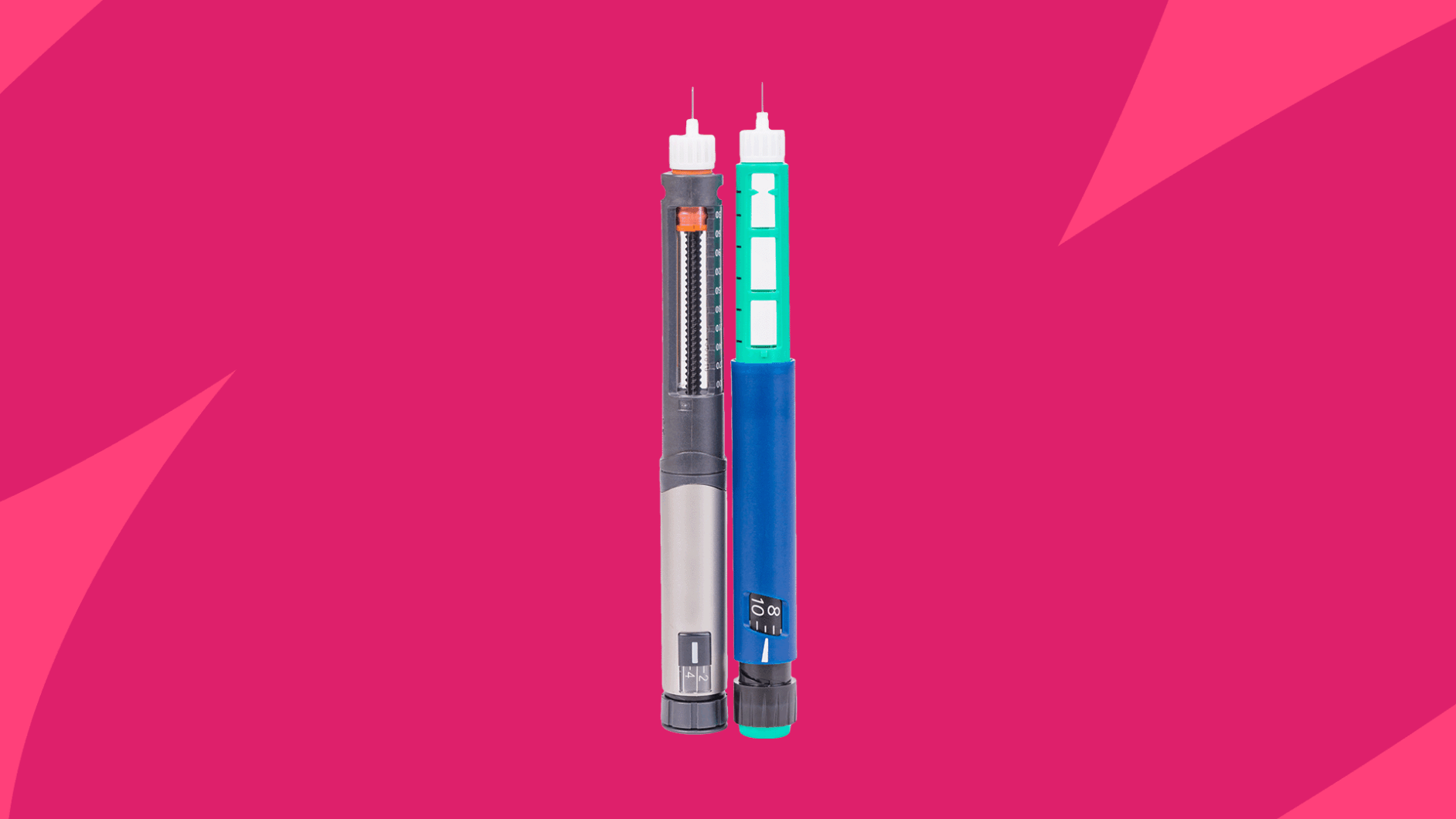
Ozempic (semaglutide) has become very popular, not only for its initial indication for treating Type 2 diabetes, but also for recently approved and off-label uses like weight loss. While it has skyrocketed in popularity, it’s not necessarily for everyone. So, who can take Ozempic, and who shouldn’t? Here are all the important details.
What is Ozempic approved to treat?
The Food and Drug Administration (FDA) initially approved Ozempic for managing high blood sugar in people with Type 2 diabetes. Since then, it’s also gained approval for reducing cardiovascular risk in adults with heart disease and Type 2 diabetes, as well as for preventing worsening kidney disease and cardiovascular death in adults with Type 2 diabetes and chronic kidney disease.
“Its primary mechanism of action is to regulate insulin release in the body, which makes sense for managing blood sugar,” says Logan G. Galbraith, MD, a physician at Invigor Medical. “However, another natural function of semaglutide in the body is to influence satiety and appetite effects that are predictable based on how the peptide works.”
Off-label uses for Ozempic
Because it helps people lose body weight, some healthcare professionals will also prescribe Ozempic for weight management. This is considered an off-label use, since it’s for a condition that doesn’t fall under the drug’s official FDA approvals. According to a study of over 17,000 people, patients taking semaglutide experienced an average weight loss of 10.2% and a reduction in waist circumference of 7.7 cm.
Yet the benefits don’t stop at weight management. “By addressing weight loss with medications like semaglutide, we are in fact addressing and protecting overall patient health,” Dr. Galbraith says. He says these benefits can include improved cholesterol and blood pressure levels, plus a reduced risk of cardiovascular events like heart attack and stroke.
The other primary off-label use for Ozempic is to treat polycystic ovarian syndrome (PCOS). A study from the Journal of Diabetes and Its Complications found that GLP-1 medications (Ozempic’s drug class) reduced body mass index (BMI), triglycerides, waist circumference, and total testosterone in people with PCOS.
Who can take Ozempic for weight loss?
If we’re sticking strictly to its FDA-approved purpose, Ozempic should treat obesity in adults over 18 who also have Type 2 diabetes. The two often go hand in hand, so it’s a fairly common diagnosis. “Many patients are great candidates for Ozempic treatment, particularly those who would benefit from weight loss, and heart/kidney protection in addition to glycemic control,” says Diana Roman, Pharm.D., assistant professor at the Marshall B. Ketchum University College of Pharmacy.
But seeing the demand for Ozempic as an obesity drug, manufacturer Novo Nordisk produced another drug with the same active ingredient that’s specifically for weight loss. It’s called Wegovy, which also has the active ingredient semaglutide but in different doses than Ozempic.
So while healthcare providers can still prescribe Ozempic for weight loss, there is a separate, officially FDA-approved option from the same manufacturer.
RELATED: When is the best time to inject Ozempic?
Who should not take Ozempic?
Having Type 2 diabetes (and potentially obesity) doesn’t automatically make someone a good candidate for Ozempic treatment. Certain medical conditions and other medications might make it an unsafe option for some.
Ozempic contraindications
“Patients with a personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2 (MEN2), Type 1 diabetes, or diabetic retinopathy should absolutely NOT take semaglutide,” says Kathryn Horton, MD, Internal Medicine Physician at Drugwatch.com.
Semaglutide research has shown that it increases the risk of thyroid tumors in laboratory animals. It’s unclear whether this risk of thyroid cancer applies to humans as well, and other studies have suggested that it might not. That’s why the FDA still issued a boxed warning on Ozempic for people who have a personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2—a condition that causes endocrine gland tumors.
“Similarly, patients with a history of pancreatitis, cholecystitis, gallstones, kidney stones, or gastroparesis should carefully weigh the risks and benefits of taking semaglutide before starting it,” Dr. Horton says. It’s also contraindicated for anyone who has a known hypersensitivity to semaglutide or any of Ozempic’s other ingredients.
Drug interactions
Taking certain medications might also preclude someone from Ozempic treatment, since there are some interactions to be aware of. Ozempic lowers blood sugar, so taking it with other medications that also lower blood sugar can lead to hypoglycemia (symptomatically low blood sugar). This includes sulfonylureas, insulin, and other diabetes drugs.
Other precautions
Some medical conditions might make a healthcare provider hesitant to prescribe Ozempic, or possibly just require additional monitoring during treatment. These conditions include:
- Gastroparesis: Per Dr. Roman, “Ozempic is not recommended in patients with gastroparesis. This is because Ozempic slows down gut motility. It would not be appropriate in a patient who already has a slow gut.”
- Pancreas issues: Ozempic can cause pancreatitis, which is an inflammation of the pancreas.
- Vision issues: It can also cause blurred vision and increase the risk of diabetic retinopathy.
- Kidney impairment: Ozempic may actually help reduce the risk of worsening kidney disease, but it has also been linked to acute kidney injury, so people with prior kidney issues might need to be cautious.
- Pregnancy or breastfeeding: It’s unknown if Ozempic affects pregnancy or passes into breast milk.
- Gallbladder issues: Ozempic has also been linked to gallstones and other gallbladder diseases.
These conditions don’t automatically disqualify you from treatment, but they might be enough to encourage your healthcare provider to consider other medications or treatment.
Side effects
Most drugs come with a risk of side effects, and they don’t necessarily preclude someone from treatment. However, some people who experience adverse effects might decide they want to discontinue Ozempic. Clinical trials show that the most common side effects of Ozempic are gastrointestinal, such as constipation, nausea, vomiting, and diarrhea. It may also cause serious side effects like pancreatitis, acute kidney injury, facial swelling, and gallstones, but these are much more rare.
It’s important to inform your healthcare provider about any side effects you experience. They may suggest an alteration in your Ozempic dose, change to a different medication, or take you off the drug completely.
RELATED: What is the maximum dose of Ozempic? | Ozempic side effects in females
How to ask your doctor for Ozempic
The best way to find out whether you can take Ozempic is to talk to your healthcare provider. They know your medical history, lifestyle, and preferences, so they can let you know if it’s a good option for you.
“This conversation is also important to tease out what the patient’s goals are by taking Ozempic and ensure they are achievable or realistic,” Dr. Horton says. “This dialogue is also an important opportunity for counseling the patient that a medication like Ozempic works best when combined with a balanced diet and regular physical activity.”
When asking your healthcare provider for Ozempic, discuss your prior weight-loss attempts, like dieting, exercising, or taking supplements or other medications. If you haven’t made other lifestyle changes to lose weight, it’s important to develop a diet and exercise plan to complement Ozempic treatment. It can also be good to create and share weight loss goals, so your healthcare provider knows your timeline and how much weight you’d like to lose. All of these details will help tailor medical advice to your specific circumstances.
There are some websites that claim to offer compounded semaglutide at lower prices than brand-name Ozempic. Compounded drugs are mixed by a pharmacy, not manufactured by the official producer, but Dr. Roman recommends against them. “These compounded products are not approved by the FDA,” she says. “Simply put, we are not certain about their content, safety, quality, or effectiveness.”
The American Diabetes Association also recommends against compounded GLP-1 medications, as does the FDA. Plus, there have been cases of counterfeit Ozempic that could contain harmful ingredients. So, it’s best to consult your healthcare provider before taking any drug, particularly one that’s not FDA approved.
- Ozempic label, Food and Drug Administration (2025)
- Long-term weight loss effects of semaglutide in obesity without diabetes in the SELECT trial, Nature Medicine (2024)
- The efficacy and safety of GLP-1 agonists in PCOS women living with obesity in promoting weight loss and hormonal regulation: A meta-analysis of randomized controlled trials, Journal of Diabetes and its Complications (2024)
- Obesity and Type 2 diabetes, National Institutes of Health (2023)
- FDA approves new drug treatment for chronic weight management, first since 2014, Food and Drug Administration (2021)
- Semaglutide injection, MedlinePlus (2025)
- Assessment of thyroid carcinogenic risk and safety profile of GLP1-RA semaglutide (Ozempic) therapy for diabetes mellitus and obesity: A systematic literature review, International Journal of Molecular Sciences (2024)
- Acute pancreatitis in a patient taking semaglutide, Cureus (2023)
- Update on semaglutide risks, American Academy of Ophthalmology (2021)
- Acute kidney injury associated with semaglutide, Kidney Medicine (2021)
- Association of glucagon-like peptide-1 receptor agonist use with risk of gallbladder and biliary diseases, JAMA Internal Medicine (2022)
- Compounded GLP-1 and dual GIP/GLP-1 receptor agonists: A statement from the American Diabetes Association, Diabetes Care (2025)
- FDA’s concerns with unapproved GLP-1 drugs used for weight loss, Food and Drug Administration (2025)