Key takeaways
One in four adults in the U.S. has a disability, many of whom require medication to manage chronic conditions, making medication management critical for avoiding dangerous errors.
The guide emphasizes the importance of working with healthcare providers to navigate medication management effectively, ensuring safe and optimal use of prescriptions for those with disabilities.
Medication labels, both prescription and over-the-counter, contain vital information such as dosage, usage instructions, and warnings, which are crucial for safe medication management.
Various strategies, including the use of technology, visual aids, and personalized healthcare consultations, can assist individuals with disabilities in managing their medications more efficiently and safely.
Even when people want to do everything they can for their health, there can be barriers that get in the way. One in every four U.S. adults has a disability, according to the Centers for Disease Control and Prevention (CDC). Of those with a disability, some may also be dealing with other medical conditions, such as diabetes.
Diabetes may be just one of the chronic conditions someone with a disability may have, and it’s likely that medication is necessary for preventing complications and improving health outcomes. This guide is designed to help people with disabilities work with their healthcare provider to navigate the medications and make the right decisions for a healthy lifestyle. With the right approach to medication management, people with disabilities can be empowered to get the most benefit from their prescriptions.
Why this guide
Medicine only works if you take it. It can sometimes be difficult to keep track of several medications that are being taken for different conditions.
If you have any questions or concerns about medications, you should always speak with your healthcare team first. Avoid skipping your medication, changing your medication dose, or changing your medication schedule. This guide is designed to provide you with more information about medication management and empower you to work with your provider to get the best treatment possible.
How to read medication labels
With any new prescription or over-the-counter medicine, it’s important to take time to completely review your medication label for vital information such as the name of the drug, the strength of the drug, the dosage of the medication, and any other details you need to know.
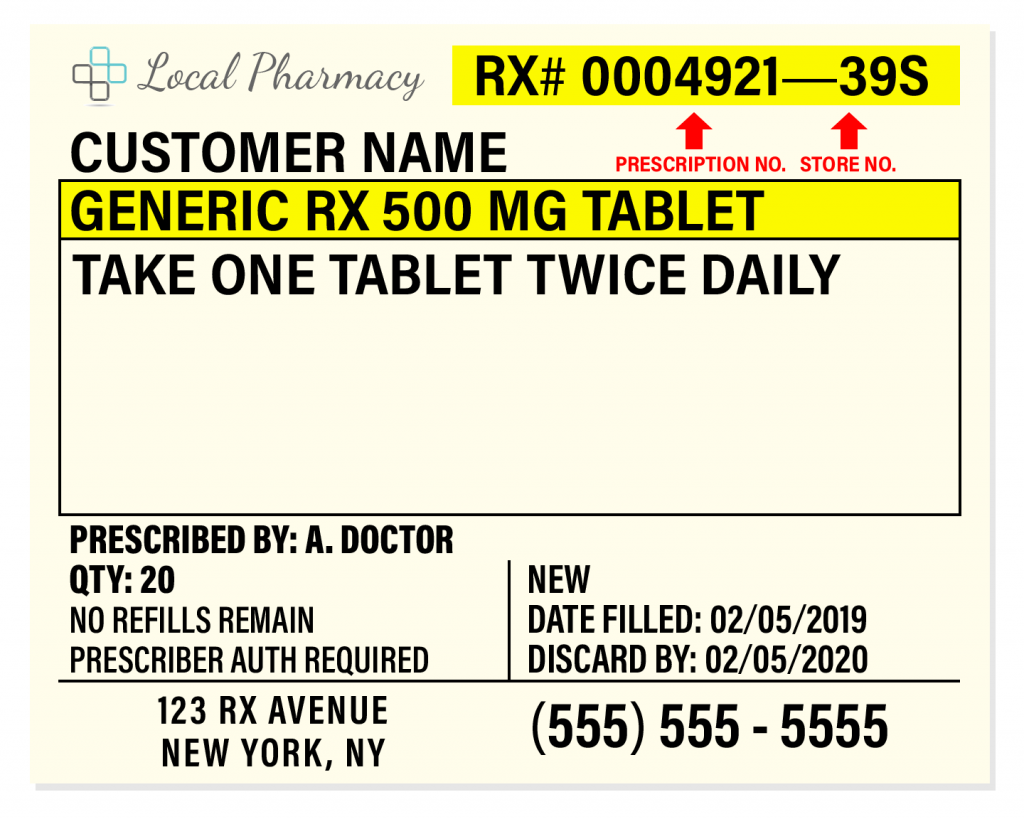
Medication labels may differ depending on the pharmacy, but they normally have eight different types of information.
- Information about the pharmacy: The name, address, and contact information for the pharmacy that filled the prescription.
- Your information: Here, you’ll find the name and address of the person to whom the medicine is prescribed.
- Information about the prescribing doctor: The doctor or other healthcare professional who wrote the prescription is listed here, along with their contact information in case you (or the pharmacy) have any questions.
- Medication name and strength: This part of the label indicates the drug’s brand name, chemical make-up, or generic name, and how strong one unit of the medication is. The strength of the medication is the amount of drug in the given dosage form and is often measured in micrograms (mcg), milligrams (mg), or grams (g). The strength of an oral solution is measured as the weight of the drug dissolved in a certain volume of solution.
- Instructions: Read these instructions carefully to learn how to take your medication. If you have any questions or concerns, be sure to ask your pharmacy or your doctor. Medication instructions usually say how to take your medicine, how often, and when. For instance, your instructions may say, “take one tablet by mouth twice a day in the morning and at night” or “apply to the affected area as needed up to five times per day.” There may also be additional precautions or important details on how to take the drug.
- Prescription information: Additional information such as the date your prescription was filled at the pharmacy, the number of pills or doses provided, how many refills you have left for your prescription, the medication’s expiration date, and an identification number your pharmacy assigned to your prescription is often included on the label..
- Drug manufacturer information: This information shows the name of the company that manufactured the medication and a physical description of the medication’s dosage form, such as a tablet, capsule, injectable solution, cream, or nasal spray.
- Federal warning statement: This is a cautionary statement that may read as, “Caution: Federal law prohibits the transfer of this drug to any person other than the patient for whom it was prescribed.” Keep in mind that you should never take someone else’s prescription medication, even if it’s been prescribed to you before. It’s not safe to take a medicine that’s not prescribed to you, as doing so may put your health at risk.
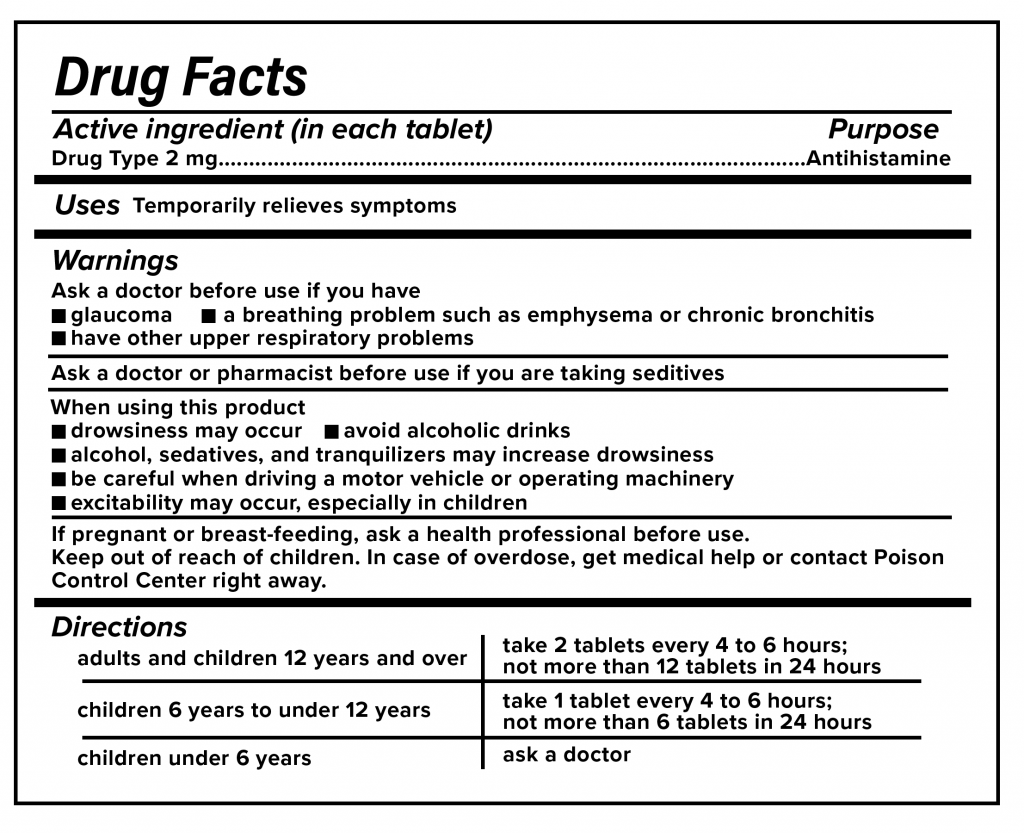
Over-the-counter medication labels, called drug facts labels, are different from prescription labels as they’re not specific to any one person. Instead, they provide information for the general public. What’s on these labels is regulated by the U.S. Food and Drug Administration (FDA), so drug facts labels generally look pretty similar to one another.
-
- Active ingredient(s): This section shows the medication’s active ingredients, along with how much of the active ingredients one dose contains.
- Uses: This section indicates the symptoms or conditions the medication is designed to prevent or treat.
- Warnings: This section lists situations when you should avoid taking the medication, possible drug interactions or side effects, any conditions that may require asking a doctor’s advice before taking the medicine, when you should stop taking the drug and see your physician, and other essential information for taking the medicine safely. Read these warnings carefully, and be sure to check with your doctor or pharmacist if you’re concerned about anything you read in this section.
- Inactive ingredients: A list of any other ingredients in the medication that don’t have therapeutic effects. Inactive ingredients may include fillers, flavoring, coloring, or preservatives.
- Purpose: The drug class of the medication is printed here. For instance, the drug may be a pain reliever or antiseptic.
- Directions: The directions outline how to take the medication. It may list different dosages by age or for different symptoms. It may also recommend that you ask your doctor for help.
- Other information: Here, you’ll find anything else the manufacturer needs you to know about the medicine. This may include directions for storing your drug.
What to do with medication label information
As you read the label on a new medication, write down any questions you plan to ask your healthcare provider. Add any new prescriptions to your medication reminder app or list to help you remember how and when to take each dose.
Remember to check with your pharmacist if you have any questions about what you read on your medication labels. If something on a label seems confusing or looks strange, it’s always a good idea to ask a healthcare professional for advice.
Your prescriptions are personalized by your healthcare provider according to the health conditions you have and your overall medical history. When determining your treatment regimen, your healthcare team will also account for your response to past treatments, any allergies you have, and other factors.
Although a friend or family member may take similar medications as you, your prescription may still work differently for you. It’s important to ask a healthcare professional for advice before taking any new medications.
Your doctor can also help you come up with strategies for managing and safely storing medications at home. Don’t hesitate to share any issues you may face with managing medications, such as forgetting to take your medication or forgetting what the medication is for. Your doctor can help guide you on how to remember to take your medications and tips for ensuring the medication works in an optimal way.
Managing your medications at home
As a patient, it’s important to remember that you’re an essential part of the healthcare team. You know what your needs are, and you’re the best person to communicate your concerns and preferences.
Some patients end up not following their doctors’ advice or skipping their prescriptions altogether. Having a disability can make it more challenging to follow your doctor’s orders.
“Patients with disabilities should ask their doctors and pharmacists for help,” says Amarish Davé, DO, a neurologist at Mercy Health in the Northern Illinois area. “Medications can sometimes be prescribed differently for individuals based on their conditions.”
According to Dr. Davé, healthcare teams can provide different treatment options to make managing medications easier. They may prescribe an extended-release formulation that you don’t have to take as often—which could allow you to take a pill once per day instead of two or three times per day. Occasionally, your doctor can switch you to an alternative medicine or eliminate certain medications completely if they’re no longer needed.
Patients can optimize how they keep track of their medications. Dr. Davé says sometimes the low-tech options work best: “Simple refrigerator lists or pill boxes can make a difference.”
RELATED: Why medication adherence matters
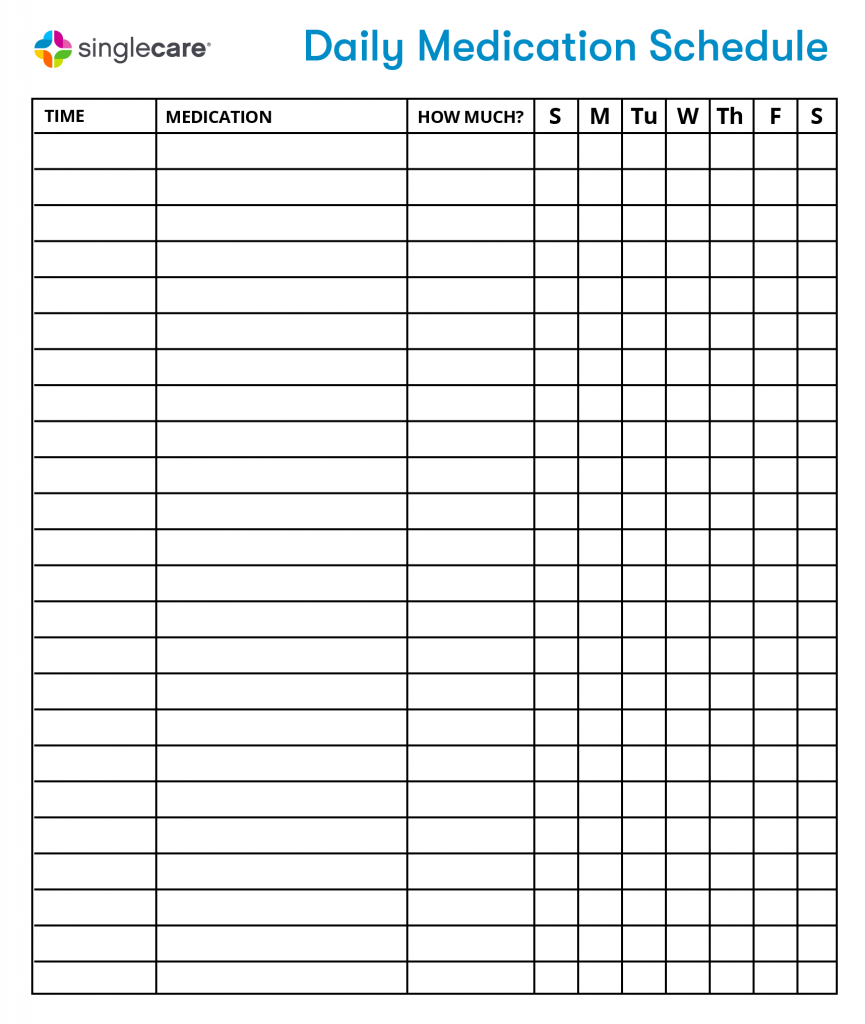
Download the Daily Medication Schedule
Although these medication strategies can be helpful for people with disabilities, it’s essential to work with your healthcare provider to find the best solutions for you. Feel free to use the tips that make sense for you and your lifestyle.
Medication strategies for people with visual impairments
Reading medication instructions and being able to clearly see and interpret labels is important. For people with visual impairments, large text sizes and cues that rely on other senses can help make it easy to read information.

Certain strategies can help serve as a starting point. You can request that your healthcare provider or pharmacist help you implement the following strategies if you have problems with vision.
- Change reading materials: For labels and important medication information, a font of at least 16 points can help with clarity and readability. Use braille labels and reading materials if needed.
- Use visual cues: You can use a large black marker to note a.m./p.m. on a bottle or write a number for how often a medicine should be taken. You could also use rubber bands or raised stickers. For example, wrap a rubber band three times around the bottle, or add three epoxy stickers to represent taking the medicine three times a day. Color-coding prescription bottles can be a helpful reminder; for example, you could use blue-colored bottles for nighttime and red-colored bottles for the morning.
- Magnification, lighting, and different labels: Ask for a different label that’s easier to read, has less glare, or is printed with better contrast. In some instances, using a magnifier or brighter lighting can make reading easier.
Auditory technology makes it easier to manage medications with limited (or no) reliance on vision.
- Talking devices: Some medical devices such as glucose meters and insulin injectors are available with audio instructions that communicate with the patient.
- Alarms and reminders: Sound-based alarms and reminders can be helpful for keeping track of medication use and remembering when to take the next dose.
- Assistive applications: Certain mobile apps or devices may be available that communicate important drug information and instructions on how to take a medication.
Lifestyle modifications and setting routines or habits can also be helpful:
- Timer caps for your pill bottles can help you remember which medication to take and when to take it.
- Taking medications at the same time every day can help make taking medications a healthy habit.
- Mentally link your medications to specific daily routines such as brushing your teeth, taking a shower, or preparing for bed.
- Use a specific shelf to organize different bottles of pills and other medications. Different shelves or compartments can be used for different medications that are taken at different times of day, for instance.
- Enlist a friend or family member to help keep you accountable and stay organized. You can also ask your doctor to recommend caregiving options to help you.
Medication information can be presented differently for patients with visual impairments, and your healthcare team should be able to make accomodations for you. You can also ask your pharmacist for suggestions and helpful tips for managing medications with a disability.
Medication management for people with a physical disability and/or mobility limitations
To start, make sure your pharmacist is aware of your disability and any concerns you have about medication management. Explain what kind of help you’re looking for or what adjustments you’ll need to safely take your medication. In some instances, a simple change by your healthcare team can make it easier to take your medicine.
- Providing non-childproof lids: Although they’re lifesaving for children, childproof lids can be tricky for people with certain physical disabilities. First, ask your pharmacist if a childproof lid is necessary for you since not all medications need them. If your medication is potentially dangerous to children or pets, you can still use a normal medication lid as long as you keep your medicine out of reach. It could be in a high cabinet, in a lockbox, or even on top of the refrigerator.
- Providing blister packs or cartridge systems: Your healthcare provider or pharmacist may recommend using a blister park or cartridge system system instead of a bottle. Popping the pill through the foil may be easier and lead to fewer lost pills in case you drop the container. Depending on your pharmacy, it may be possible to get specialized blister packs that contain each of your medications for a specific time, making management as easy as remembering which pack to pull at specific hours.
- Adjusting refills: If you have a mobility limitation or find it challenging to get to the pharmacy, ask your pharmacist or your healthcare provider about the possibility of getting refills early, receiving larger refills, or making another adjustment, so you don’t have to make as many trips to the pharmacy.
- Prescription delivery: Getting your prescriptions by mail or delivered to your door may be helpful if mobility is a challenge. Many pharmacies have convenient delivery programs. Just call and ask.
For patients with physical limitations, keep the following in mind:
- Reminder systems should be easy to use comfortably. Some pillboxes and organizers have lids that are hard to open and should probably be avoided.
- If placing medication in a hard-to-reach location isn’t possible, consider keeping drugs stored in a locked box or room to keep them from children and pets. This way, medicine is safely stored while also being accessible.
- If you have more than one medication to refill, talk to your doctor and pharmacist about having everything ready on the same day or delivered in the same shipment.
Whenever you travel to get your prescriptions, make the most of the trip. If it’s a challenge to write down questions you have for your pharmacist, consider using a recorder or an app on your smartphone. Some pharmacies have refill requests integrated into their store apps, so you can quickly ask for a refill with the press of a button.
Medication management for people with intellectual disabilities
Patients with intellectual disabilities may also need assistance with their medication.
These tips can help you manage your prescriptions more effectively if you have intellectual disabilities.
- Ask for a consultation: If you need it, ask your pharmacist for a special consultation to go over information about your medications. While it’s not always possible to get a comprehensive consultation during busy times of the day, you can schedule a medication therapy management session at a different day or time.
- Establish a preferred method of communication and learning: Let your doctor or pharmacist know how you communicate best. For instance, visual communication through pictures may be the best way for you to learn and understand information.
- Bring information home: Ask for information to bring home in a format that works for you. You might decide to take notes or request an easy-to-read medication guide or information pamphlet.
- Request a follow-up session: If you have further questions about your medications after a consultation, ask for a follow-up session with your pharmacist. They can help review and go over any other concerns you may have.
- Get the medication in a different form: Some adults with intellectual disabilities may have trouble taking pills. If swallowing pills presents a barrier to taking a medication regularly, ask the pharmacist if the medicine is available as a liquid or dissolvable tablet. A healthcare provider may also offer sprays or gels that prep the throat for easier swallowing of certain medications.
- Ask for assistance if your client, loved one, or friend refuses to take medication: Caregivers sometimes have to deal with medication refusal from the person they’re caring for. Try to find out why this is happening. Some patients don’t like swallowing pills, or they may be confused or afraid. Others may feel angry, rushed, or frustrated. If you’re taking care of someone who refuses to take his or her medicine, take a short break, make sure the surroundings are calm, and try again. If they continue to refuse to take their medication, talk to the prescribing healthcare provider or pharmacist.
Feeling confused or being afraid are common barriers to taking medication. If you are a caregiver, take the time to understand what interventions would help the most.
Tips for effective medication management as the caregiver of a person with a disability
Let’s talk about how caregivers can practice effective medication management. If you’re a professional caregiver, then you likely know that having the right strategies can help make your job a little easier. Targeted interventions can help people with disabilities live healthier, more independent lives. You can provide better care to your client and save your sanity by using some of these tips.
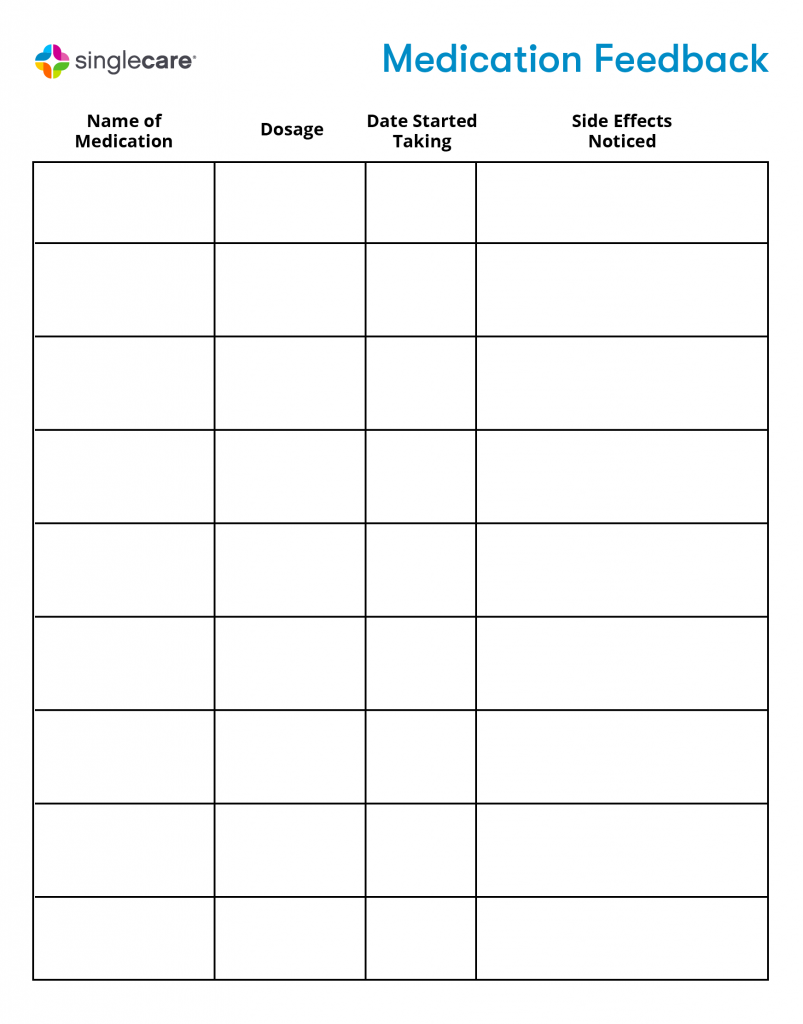
- Create and manage a medication list: If you don’t have one already, start a comprehensive list of all the medications your client is taking. Include over-the-counter drugs, prescription medications, and herbal supplements. A multivitamin or supplement can sometimes interact with other medications being taken, so be sure to write down and keep track of all medications.
- Read the labels closely: Understand the prescription and drug facts labels for the medicines your client takes. Look at possible side effects, warnings, and precautions linked to taking the medication. Have regular checkups with the prescribing healthcare provider or pharmacist to go over current medications and ensure there are no potential harmful drug interactions.
- Ask the right questions: On your client’s behalf, you can ask their healthcare provider questions to make sure your client is getting the most from their medicine.
- Why is this medication prescribed?
- How does this medication help the patient’s condition?
- How can the patient expect to feel while on this medication?
- Is this medication appropriate for the patient’s age?
- What side effects can this medication cause?
- Be consistent: Administer medication at the same time every day.
- Track dosage: Keep track of when you give a dose, which medications you give, and how much. Use a medication calendar to keep track of when you gave a certain medication.
- Create timers: Use alerts and timers, or use a pill reminder app to help you regularly administer doses. Your timer can be one that’s audible and obvious to your client or loved one so that they get in the habit of knowing it’s time for their medications. In some cases, it may be better to have silent notifications, so that you have time to prepare the medication doses and have everything ready for a client who may not be eager to take their medications. Seek to understand how timers may reduce or cause stress to your client so you can use the best strategy for managing their medications.
Download the Medication Feedback Form
Reviewing your medication list and medication safety
On a regular basis, meet with your doctor or pharmacist to review your medication list. If you’re a caregiver of a client with a disability, urge your client to attend a medication therapy management session. A healthcare provider or pharmacist can review all medications being taken and address any concerns about them. This is your opportunity to advocate for yourself or for your client and ensure that the medications being taken are the best options.
Since many clinics and hospital systems have moved completely to electronic patient files, it’s now easier than ever to communicate medication issues and changes between providers within the same system. After every appointment or consult, you should be able to ask for a printout of all current medications and their dosages. This information is usually given to patients with new prescriptions, along with next steps for future appointments.
Ask your healthcare provider if they have an online patient portal. You can sign onto the portal to check all current prescriptions and ask questions as needed. With an online portal, you can also see lab results, notes from appointments, and future appointment dates.
As always, if you have any questions or concerns about your medication, do not hesitate to ask your healthcare team. Be an empowered patient or advocate. Learn how to take medications safely and effectively.