Compare Mirena alternatives | Annovera | Depo-SubQ Provera 104 | Nexplanon | Twirla | Xulane | Natural alternatives | How to switch meds
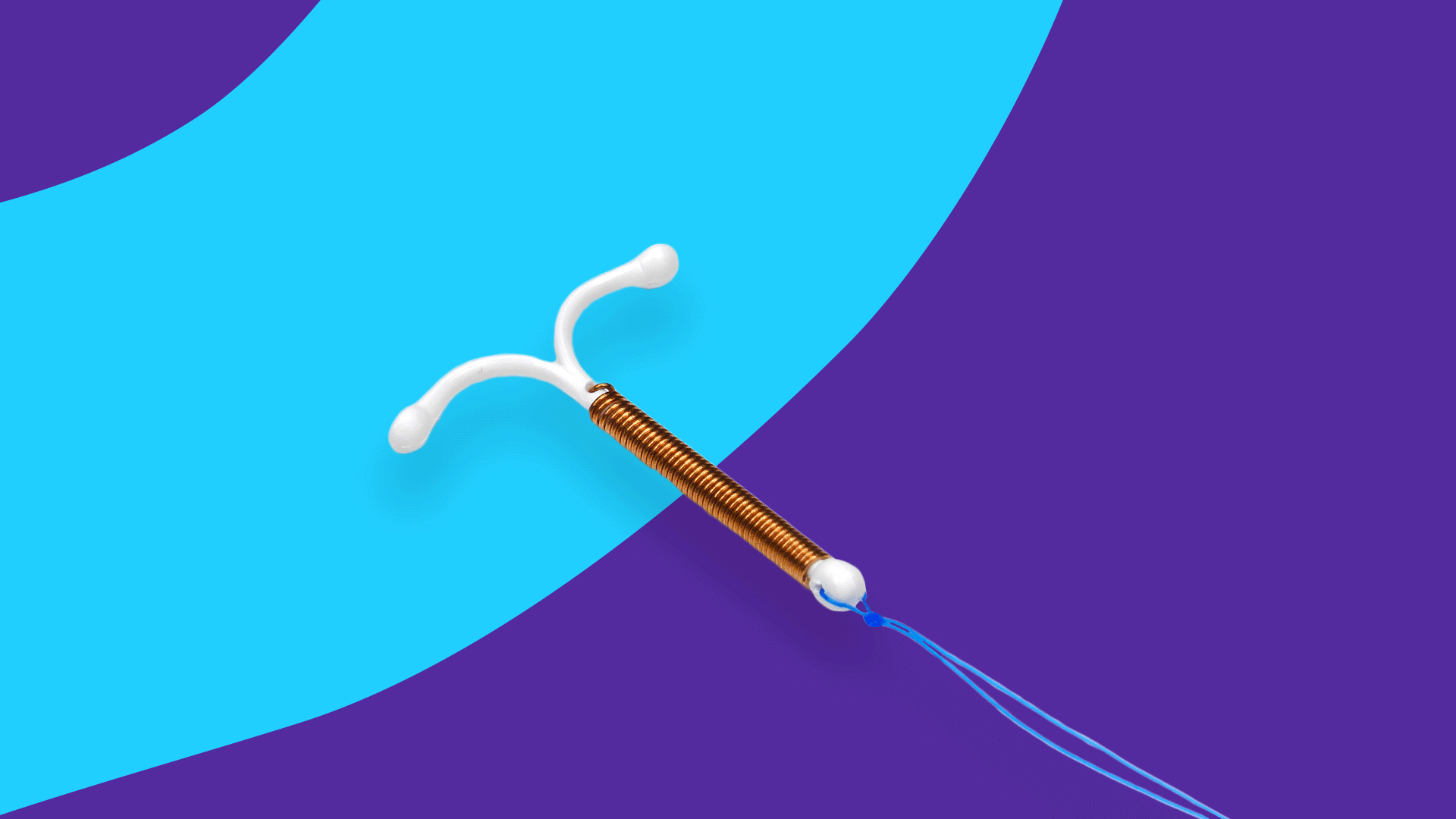
The decision to avoid pregnancy is complex—but once that decision has been, you are faced with a plethora of options with ways to uphold it. Hormonal birth control comes in many forms—from pills, injections, patches, subdermal implants, to intrauterine devices (IUDs). The type of hormonal contraceptive to use is often up to preference, and an IUD, like Mirena, is an option for someone without any risk factors for the use of a combination hormonal contraceptive. It’s also a good option for someone that will not remember to take a daily pill reliably, or knows they want long-term contraception.
Hormonal contraceptives are not always taken to avoid pregnancy; they are also considered a first-line option to treat endometriosis-associated pain because they shrink endometrial tissue. Hormonal contraception may also be beneficial in women who experience dysmenorrhea, or menstruation with painful abdominal cramps. Mirena may be particularly helpful in patients suffering from dysmenorrhea and menorrhagia, which is heavy menstrual bleeding. Hormonal contraception can even protect against pelvic inflammatory disease (PID) and ectopic pregnancy.
Mirena IUD contains only a progesterone hormone, levonorgestrel. Combination hormonal contraceptives, which also include an estrogen, are often preferred over progestin-only products since side effects like headaches, irregular vaginal bleeding, weight gain, and mood changes are more common with those products. However, these combination hormonal products come with risks in certain higher-risk patients due to underlying comorbid conditions. For many reasons, a person may benefit from Mirena alternatives—be it different IUDs, or different forms of hormonal contraceptives altogether.
Here we will discuss Mirena and the type of patient for which it is a good option for birth control, as well as scenarios in which other hormonal contraceptive alternatives other than birth control pills might be a better option. It is important to point out that hormonal birth control methods never prevent sexually transmitted infections (STIs).
What can I take in place of Mirena?
There are birth control options available other than hormonal IUDs like Mirena. These alternative forms of contraception include other types of IUDs and other classes of reversible hormonal contraception, such as injectable, topical, and oral formulations. These options may be more suitable for certain individuals due to their different routes of administration, side effect profiles, drug interactions, and efficacy in preventing pregnancy.
Compare Mirena alternatives |
|||
|---|---|---|---|
| Drug name | Uses | Dosage | Savings options |
| Mirena
(levonorgestrel) |
Contraceptive | Intrauterine device with levonorgestrel 20 mcg/day for up to 5 years; must be removed after 8 years | Mirena coupons |
| Annovera
(ethinyl estradiol/segesterone) |
Contraceptive | Ethinyl estradiol 13 mcg/day; segesterone acetate 150 mcg/day
Vaginal ring inserted and left in for 3 weeks and removed for 1 week |
Annovera coupons |
| Depo-SubQ Provera 104 (medroxyprogesterone acetate) | Contraceptive | 0.65 mL (104 mg) medroxyprogesterone acetate subcutaneous injection into the anterior thigh or abdomen, once every 3 months (12 to 14 weeks) | Depo-SubQ Provera 104 coupons |
| Nexplanon (etonogestrel) | Contraceptive | Etonogestrel 60 to 70 mcg/day – reduces annually, must be removed by end of the third year
Implanted subdermally at the inner side of the non-dominant arm |
Nexplanon coupons |
| Nuvaring
(ethinyl estradiol/etonogestrel) |
Contraceptive | Ethinyl estradiol 15 mcg/day; etonogestrel 0.12 mg/day
Vaginal ring inserted and left in for 3 weeks then removed for 1 week |
Nuvaring coupons |
| Twirla
(ethinyl estradiol/ levonorgestrel) |
Contraceptive | Ethinyl estradiol 30 mcg/day; levonorgestrel 120 mcg/day
Transdermal patch applied weekly (for 3 weeks, then week 4 is patch free) |
Twirla coupons |
| Xulane
(ethinyl estradiol/ norelgestromin) |
Contraceptive | Ethinyl estradiol 35 mcg/day; norelgestromin 150 mcg/day
Transdermal patch applied weekly (for 3 weeks, then week 4 is patch free) |
Xulane coupons |
Other alternatives to Mirena
Combination birth control pills
- Monophasic
- Biphasic
- Triphasic
- Quadriphasic
Progestin-only pills
- Drospirenone
- Slynd
- Camila
- Deblitane
- Errin
- Heather
- Incassia
- Jencycla
- Lyleq
- Nora-BE
- Norethindrone 0.35mg
- Norlyda
- Sharobel
Emergency contraception
- Aftera
- EContra One Step
- My Way
- Plan B One-Step
- Ella
Other contraceptives
- Depo-Provera CI
- Kyleena
- Liletta
- EluRyng
- Paragard
- Phexxi
- Skyla
- Zafemy
Top 5 Mirena alternatives
The following are some of the most common alternatives to Mirena.
1. Annovera
Annovera is a vaginal ring combination hormonal contraceptive which can be inserted and left in for three weeks and then removed for one week. The ring can be reused for up to 13 cycles, or a full year of use, but should be washed prior to reinsertion. Hormonal contraceptive rings like Annovera have the advantage over other combination hormonal contraception of avoiding difficulty with daily or weekly use; its advantage over an IUD like Mirena is the user control it offers as easily reversible contraception since an IUD must be removed by a healthcare professional.
2. Depo-SubQ Provera 104
Like an IUD, depot medroxyprogesterone is a good hormonal contraceptive option in someone at risk for non-adherence since it is long-acting. It is also a good option for someone that knows they do not want to conceive within the next year; return to ovulation and fertility may be delayed in those taking Depo-SubQ Provera 104 since it can take from two months to over a year to completely clear progestin from the body. Depo-SubQ Provera 104, as a progestin-only containing birth control like Mirena, is also a preferred type for women greater than 35 years old who smoke and who have other comorbidities like high blood pressure or an increased risk of thrombosis. Certain medications known as CYP3A4 inducers (e.g., phenytoin, carbamazepine, some HIV drugs, topiramate, rifampin, St. John’s wort) induce the metabolism of estrogen and therefore could potentially decrease the efficacy of hormonal contraceptives containing it. In patients taking a CYP3A4 inducer, depot medroxyprogesterone is a preferred hormonal contraceptive.
3. Nexplanon (etonogestrel)
Like an IUD, Nexplanon must be both inserted and removed by a healthcare professional. Nexplanon is implanted subdermally just under the skin at the inner side of the non-dominant arm, where it can remain for three years. Etonogestrel, the active ingredient of Nexplanon, is poorly metabolized in patients with liver disease and should be avoided in this patient population. This product should be used cautiously in patients who are overweight as it may be less effective due to lower serum concentrations of the active ingredient.
4. Twirla (ethinyl estradiol and levonorgestrel)
Abnormal uterine bleeding (AUB) is a women’s health issue referring to heavy menstrual bleeding. Estrogen-progestin combination contraceptives are first-line management for AUB since they can prevent heavy periods. Twirla is a transdermal patch containing both an estrogen and progestin. This patch is applied weekly for three weeks (week 4 is patch-free), offering the potential benefit of improved compliance. Effectiveness is reduced in females with a body mass index (BMI) greater than or equal to 25 kg/m2; it is contraindicated in females with a BMI greater than or equal to 30 kg/m2 due to the risk of venous thromboembolism.
5. Xulane (ethinyl estradiol and norelgestromin)
Xulane is another option for a combination hormonal contraceptive transdermal patch applied weekly for three weeks (week 4 is patch-free). The transdermal patch may be a good option for patients who have difficulty swallowing pills. In 2020, the FDA labeled this patch as contraindicated in females with a BMI greater than or equal to 30kg/m2 based on the concern for elevated venous thromboembolism (VTE) risk in this population. A disadvantage of transdermal patches over an IUD includes the possibility of the patch not sticking well or falling off.
Natural alternatives to Mirena
Non-hormonal forms of birth control are available, and range from barrier methods (e.g., male and female condoms), copper IUDs (ParaGard), and forms of natural family planning. Natural family planning requires identification of the signs and symptoms of ovulation and fertility during a menstrual cycle to either plan or avoid pregnancy, including monitoring and recording the length of the menstrual cycle, daily readings of body temperature, and changes to cervical mucus secretions. When performed correctly, its failure rate is similar to hormonal and barrier contraceptive methods. The lactational amenorrhea method (LAM) is another form of natural contraception, as women are unlikely to ovulate or have any periods when exclusively breastfeeding. The probability of pregnancy following this method is also similar to hormonal and barrier contraceptive methods. Phexxi is a vaginal gel that is non-hormonal, containing a combination of lactic acid, citric acid, and potassium bitartrate—one applicatorful up to one before each episode of vaginal intercourse (can be used during menstrual cycle).
How to switch to a Mirena alternative
When switching from Mirena to a different contraceptive, the IUD removal should occur during the first seven days of a menstrual cycle, and the new therapy should then begin. If IUD removal does not occur at that time, or if you experience irregular menstrual cycles or no cycles, the new method should start at least seven days before the IUD is removed. If the new method is not initiated at that time, a backup barrier contraceptive method should be used for the seven days after the IUD is removed if abstention is not possible.
When switching from an oral, transdermal, or vaginal hormonal contraceptive to Mirena, IUD insertion can occur anytime—including the hormone-free interval of the previous method. If Mirena is inserted during active use of the previous method, the previous method should be continued for seven days after Mirena’s insertion or until the end of the current menstrual cycle. If using continuous hormonal contraception, continue the previous contraceptive method for seven days past Mirena’s insertion. If switching to Mirena from an injectable progestin, Mirena can again be inserted at any time. If Mirena is inserted more than 13 weeks after the last injection, a backup barrier contraceptive method should be used for seven days. If switching from an implant or a different intrauterine system (such as a copper IUD), Mirena can be inserted on the same day the implant or intrauterine system is removed, at any time during the menstrual cycle.
Given the complexities of making changes, medication changes should be discussed in detail with healthcare providers to obtain the best medical advice.