You have a lot of options when it comes to choosing a birth control method. One that ranks high among users is the IUD or intrauterine device. The IUD is a small, T-shaped device that your doctor or healthcare provider inserts into your uterus to prevent pregnancy. An intrauterine device comes in two types: hormonal IUDs and non-hormonal IUDs. They both work to prevent pregnancy but in different ways.
If you’re looking for a long-acting reversible contraception (LARC) method that is also considered effective and safe for most women, consider trying an IUD.
What is IUD birth control?
The IUD is a small intrauterine contraceptive device that your doctor or healthcare provider inserts inside your uterus to prevent pregnancy. There are two types of IUDs available in the United States. One is a hormonal IUD that releases the hormone progestin, and the other is a non-hormonal or copper-coated IUD. They are both FDA approved.
The hormonal IUDs available in the United States include Mirena, Liletta, Skyla, and Kyleena.
If you opt for the non-hormonal method, the only FDA-approved option in the United States is ParaGard.
How does an IUD work?
Both the hormonal IUD and copper IUD prevent pregnancy by preventing the sperm from reaching the egg. How they do this is what sets them apart.
Hormonal IUD
Hormonal IUDs are a tiny T-shaped piece of flexible plastic that goes inside your uterus. They work to prevent pregnancy by releasing small amounts of the hormone progestin into your body. When a hormonal IUD releases progestin, your cervical mucus gets thicker. This thicker cervical mucus slows the sperm’s movement preventing it from meeting up with an egg to fertilize it. Hormonal IUDs also keep the uterine lining very thin, which will prevent a fertilized egg from implanting in the uterus.
Some progestin-based IUDs can also prevent ovulation from occurring by stopping the eggs from leaving your ovaries. When this happens, the sperm has no egg to meet up with and pregnancy can be prevented.
In addition to its typical use as an effective birth control method, hormonal IUDs may also reduce premenstrual symptoms like cramping and make period bleeding lighter. Some women may stop having a period altogether, while others may experience irregular bleeding or spotting during the first few months.
Non-hormonal IUD
The non-hormonal IUD uses copper to prevent pregnancy, which the sperm cells do not like. The copper causes the sperm to change the way they move, preventing them from swimming to an egg and fertilizing it. If the egg is not fertilized, it cannot implant in the uterine wall, which means pregnancy cannot happen.
Unlike the hormonal IUD, the copper IUD is only available in one brand, which is called the Paragard IUD or copper T IUD. However, this hormone-free IUD works longer to prevent pregnancy. Unless you experience problems with the Paragard, you can leave it in for up to 10 years.
Chances of pregnancy
The chances of getting pregnant with both types of IUDs are low. According to the American College of Obstetricians and Gynecologists (ACOG), the IUD, which is considered a long-acting reversible contraception method, is one of the most effective birth control options available. During the first year of use, the ACOG says fewer than 1 in 100 women with an IUD will get pregnant.
Paragard, the copper IUD, can prevent pregnancy right away after insertion. However, it’s important to note that Mirena, Kyleena, Liletta, and Skyla—the hormonal IUDs—only prevent pregnancy immediately after insertion if your doctor placed it during the first seven days of your menstrual cycle. Otherwise, they begin working seven days after insertion, according to Planned Parenthood.
Neither type of IUD will protect you from sexually transmitted infections, or STIs. For increased protection, ask your partner to wear a condom.
IUDs as emergency contraception
If inserted within five days of unprotected sex, the Paragard (copper) IUD is considered a form of emergency contraception. However, the hormonal IUDs cannot be used as emergency contraception.
IUD insertion and removal
Your doctor or healthcare provider will perform IUD insertion and removal in their office. Both procedures are relatively quick and only cause minor discomfort.
IUD insertion
Before placing an IUD, your doctor will review your medical history and perform a pelvic exam. You can have an IUD inserted any time during your monthly cycle. To insert the IUD, your doctor will first put a speculum into your vagina. They will use a tool to guide the device through your vagina and the cervix and into the uterus.
“IUDs are fairly easy to insert in the majority of patients,” says G. Thomas Ruiz, MD, OB-GYN Lead at MemorialCare Orange Coast Medical Center.
The IUD has strings to help with the removal process. These thin plastic threads should not bother you. Your partner may feel these strings during sex in very rare cases, but it is highly unlikely. Your doctor may be able to trim the strings.
You should periodically check the length and position of the strings to make sure that they haven’t changed. Strings that are suddenly shorter or missing may indicate that the IUD has moved out of position. You should call your doctor with any questions or concerns.
Typically, the only discomfort during IUD insertion is moderate cramping. You can take an over-the-counter pain relief medication before or after to reduce the pain. If you have a low pain tolerance, Dr. Ruiz says your doctor can use a local anesthetic block to lessen the uterine cramping. “It is on rare occasions that one abandons the procedure due to severe pain,” Dr. Ruiz says.
After the procedure, you may feel pain and cramping, so take it easy for a few days. Your doctor may recommend over-the-counter pain relievers until the pain subsides.
In rare cases, an IUD can fall out. If this happens, see your doctor right away.
IUD removal
When you’re ready to stop using an IUD, your doctor can remove it any time during your menstrual cycle.
Removing an IUD is quick and simple. Your doctor will use an instrument to grasp the strings, which allows them to pull the IUD from your cervix. It typically takes a few minutes, and you may only experience mild cramping and bleeding. If this does not go away within a few days, call your doctor.
If you’re replacing an IUD, your doctor can insert the new IUD immediately after removing the old one. They can do this during the same office visit, provided there are no complications. You should never pull on the strings or attempt to remove an IUD yourself.
After removal, you can expect your period to return to the way it was before the IUD. But this may take a few months. You can also get pregnant after removal. So, make sure to use another birth control method if you don’t want to get pregnant.
IUD side effects
All birth control options come with side effects. Fortunately, most of the side effects from an IUD are mild and go away or get less noticeable within a few months. Here are some of the more common side effects you might experience with IUD use.
Copper IUD side effects include:
- Heavier and longer-lasting periods
- More severe menstrual cramping
- Irregular periods
- Spotting between periods
- Pain and cramping with IUD insertion
Hormonal IUD side effects include:
- Bloating
- Frequent spotting or more days of bleeding in the first month.
- Spotting between periods.
- Irregular periods
- Menstrual bleeding may stop completely altogether
- Headache
- Nausea
- Breast tenderness
- Mood changes
- Pain and cramping with IUD insertion
Some users are worried about weight gain with an IUD. The good news? The copper IUD does not cause weight gain. However, a small percentage of people report minor weight gain with a hormonal IUD, like Mirena, due to the release of progestin. But it’s unclear if this is due to the progestin or other lifestyle factors. If you have concerns about weight gain, talk to your doctor.
What are the disadvantages of the IUD?
The IUD is a popular form of birth control, but that doesn’t mean it’s right for everyone. According to Kecia Gaither, MD, a board-certified OB-GYN and maternal fetal medicine specialist at NYC Health + Hospitals/Lincoln, women with the following conditions should not use an IUD:
- Do not use a copper IUD (non-hormonal) if you have a copper allergy or Wilson’s disease, which is a rare disorder that causes copper to accumulate in vital organs like the brain and liver.
- Do not use a hormonal-IUD if you have a history of breast cancer.
- Do not use a hormonal IUD or non-hormonal IUD if you have cancer of the cervix or uterus, AIDS, intermenstrual bleeding, or liver disease.
- Women with active or acute pelvic inflammatory disease should not have an IUD placed until the infection has resolved. The doctor may screen you for an infection before inserting the IUD.
There are also instances when an IUD is not the best option, but it can still work.
Talk to your doctor if you have heavy menstrual bleeding. They may advise against using a copper IUD since it can cause heavier periods and cramping.
For some people, heavy bleeding and cramping gets better after six months, but for others, it continues until removal of the IUD. If you can wait it out for the initial period of three to six months, you may find that the symptoms decrease enough to make it tolerable.
Additionally, Dr. Ruiz explains that IUDs are contraindicated in women with abnormal uterine anatomy or an abnormal uterine cavity. “IUDs are also not recommended in someone with abnormal uterine bleeding unless they have had an endometrial evaluation by hysteroscopy or endometrial biopsy,” Dr. Ruiz says. “That evaluation may include a pelvic ultrasound.”.
And in rare cases, there is a small increased risk of pelvic inflammatory disease when using an IUD. According to the ACOG, that risk is less than 1% or women regardless of age or IUD type. That said, the risk of developing pelvic inflammatory disease is most common during the first three weeks after your doctor places the IUD in your uterus.
According to the ACOG, the hormonal and non-hormonal IUDs do not protect you from sexually transmitted infections. Having unprotected sex puts you at a higher risk of contracting a sexually transmitted infection such as gonorrhea, chlamydia, genital herpes, HPV, and HIV.
If you have any questions or concerns, talk to your doctor or healthcare provider. They can help you decide if an IUD is the right birth control method for you.
What are the advantages of IUD birth control?
There are several advantages to both the hormonal IUD and non-hormonal IUD. The first one, Dr. Ruiz says, is the length of time they work.
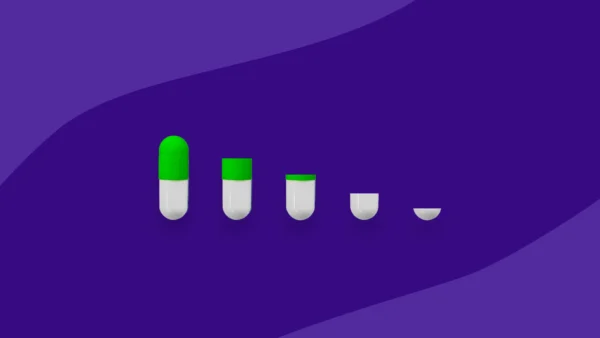
Depending on the system or type of IUD you choose, Dr. Ruiz says an IUD can stay in place and continue to work anywhere from three to 10 years. More specifically, the hormonal IUDs typically work for three to six years. And the copper IUD prevents pregnancy for up to 10 years.
The other positive is the high degree of effectiveness. “The IUD has less than 1% failure rate,” Dr. Ruiz says. Plus, since the IUD is always in place, there is no forgetting to take birth control pills, put on a patch, or see your doctor for shots.
The progestin IUDs have the additional benefit of less or no menstrual blood flow for the duration the device is in place. And copper IUDs offer a non-hormonal method for those who do not want a hormonal contraceptive.
Dr. Ruiz also points to the usefulness of progestin IUDs in women with heavier painful menses. “Within three to six months of insertion up to 50% will not have menstrual bleeding, and the other 50% will have lighter, less painful and less frequent uterine bleeding,” he says. If you do experience menstrual bleeding, it is still safe to use a tampon.
If you want to get pregnant, the IUD is an effective form of birth control to use for family planning. The IUD is a reversible form of birth control, which means it has the benefit of immediate return of fertility once it is removed. Fertility will typically return to what is normal for you.
How to get an IUD
Your doctor or healthcare provider can help you determine if an IUD is right for you. Some insurance plans cover birth control, so make sure to call before a procedure to determine eligibility. If you live near a community clinic specializing in women’s health, they may offer IUD insertion for free or at a discount.
The Affordable Care Act mandates that insurance plans cover contraceptive methods. But changes to the act may affect your eligibility for free or reduced coverage. Always check with your insurance to determine your IUDs cost. If you need assistance paying for an IUD or other birth control options such as the Depo-Provera shot, the birth control pill, and the birth control patch, be sure to compare prices on Singlecare.