Have you ever taken an over-the-counter analgesic (such as Tylenol, Advil, or Aleve) after a night of drinking to avoid or treat an alcohol-induced headache? You might want to reconsider that practice. Otherwise, you could find yourself dealing with side effects much more serious than the typical hangover—problems like ulcers, stomach bleeding, liver damage, kidney damage, and more—from mixing painkillers and alcohol.
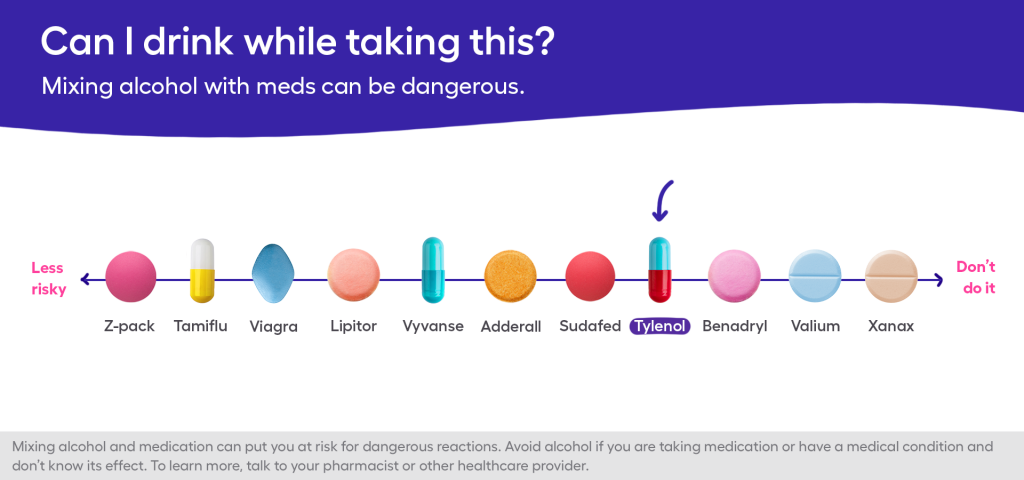
“People need to be aware that alcohol is a drug,” says Anna Lembke, MD, director of addiction medicine at Stanford University School of Medicine in Palo Alto, California. “And using alcohol in combination with any other drugs, including OTC painkillers, can exacerbate side effects or lead to drug-drug interactions.”
Tylenol and alcohol
Acetaminophen (better known under by the brand name Tylenol), for example, is well-known for its potential to cause liver damage. So is alcohol. And, the risk of damage increases when the two are mixed, according to the Food and Drug Administration (FDA).
“Alcohol and Tylenol in combination tax the liver—and the combination can be cumulative and synergistic, in a bad way, over time,” Dr. Lembke says.
Ibuprofen and alcohol
Nonsteroidal anti-inflammatory drugs (NSAIDS), like ibuprofen and naproxen, aren’t any better, says Heather Free, Pharm.D., a pharmacist in Columbus, Ohio, and spokesperson for the American Pharmacists Association. Taking ibuprofen and other NSAIDS alone can damage the stomach and increase your chances of gastrointestinal bleeding and/or getting an ulcer. Combining ibuprofen and alcohol amplifies the danger, she says. Furthermore, if you are already at risk for kidney problems (because of diabetes or family history of kidney disease), drinking alcohol while taking ibuprofen is even more precarious.
Is it ever safe to mix painkillers and alcohol?
So does all of this mean that you should never, ever take pain medication for a headache after having a drink or two? Not exactly. The problems occur when alcohol is consumed alongside painkillers regularly, Dr. Lembke explains. “If it is a small amount of alcohol and [you are] taking the painkiller as indicated on the bottle, it is generally not a problem,” she says. So, a moderate amount of alcohol and the recommended dose of pain medication should be safe on occasion as long as you are not taking other medications that might interact with alcohol.
What pain reliever can I take with alcohol?
In other words, it’s fairly safe to occasionally take a low dose of ibuprofen, acetaminophen, or naproxen if you’ve had a small amount of alcohol. However, because of the potential for long-term consequences, it is still prudent to avoid mixing painkillers with alcohol, Drs. Lembke and Free both emphasize.
“Repeated use will just progress the damage, making it difficult for the body to rebound back,” Dr. Free says. Instead, she advises rehydrating your body with water and plenty of electrolytes as treatment options for a hangover. And Dr. Lembke says it is better to just avoid drinking to the point of needing a painkiller altogether.
RELATED: 14 hangover cures that work
“If you are drinking so much that you have a hangover, you might want to look at your drinking habits,” she says. “Because if you have had enough that you have a hangover, you have had too much.”
The general rule of thumb for safe alcohol consumption, she says, is no more than seven drinks per week and definitely no more than three drinks on any one occasion. “Anything above that is considered risky drinking and is associated with all sorts of adverse health outcomes,” she says.
And while Dr. Lembke says it would be very surprising for a related medical emergency to occur if you are following these guidelines and don’t have any other risk factors, she also urges people to see a doctor right away for serious side effects like abdominal or stomach pain, altered consciousness, or jaundice. All are signs of an alcohol-related injury or a potentially dangerous drug-drug interaction.











