Gluten intolerance symptoms: What are the early signs of gluten intolerance?
Overview: What does gluten intolerance feel like?
Gluten-associated disorders comprise a spectrum of illnesses. The most serious is celiac disease (gluten-sensitive enteropathy), a condition in which gluten sensitivity provokes an immune response that also causes intestinal damage. Non-celiac gluten sensitivity (NCGS) is also an immune response to gluten-containing foods, but there is no damage to the intestinal walls. However, healthcare professionals aren’t really certain what NCGS is or if it is even caused by gluten itself. It may actually be due to other substances in cereal grains. When some people say “gluten intolerance,” they sometimes only mean NCGS rather than other gluten-associated disorders, but others may use the term more broadly. Still, both conditions can be considered forms of gluten intolerance.
It’s important to know the difference. People are diagnosed with NCGS only when blood tests and biopsies show no evidence of celiac disease. So the two conditions are very similar: they have the same digestive system complaints, the same triggers, and the same treatment. Both can cause diarrhea and other gastrointestinal problems like bloating, gas, and abdominal pain, in addition to tiredness or headaches. People with celiac disease, however, may eventually experience problems throughout the body because of malnutrition and the immune system’s reaction to gluten. Fortunately, for both conditions, symptoms resolve fairly quickly once gluten-containing products are removed from the diet.
Key takeaways:
Gluten intolerance is a health condition that can affect anyone, regardless of age, sex, race, or ethnicity.
Early signs of gluten intolerance include low energy, diarrhea, bloating, and other digestive system complaints.
Serious symptoms, such as anemia, muscle weakness, bleeding, unexplained weight loss, or seizures, may require immediate medical attention. These are all serious symptoms of celiac disease, a potentially serious form of gluten intolerance.
Gluten intolerance is triggered by gluten exposure from consuming gluten-containing foods, though heredity may be a related factor. You may be at risk for non-celiac gluten sensitivity if you already have food allergies or intolerances.
You may be at risk for developing celiac disease if you have Type 1 diabetes, autoimmune disorders, or are descended from northern Europeans. The risk is highest in people who have an immediate family member with celiac disease.
Gluten intolerance usually requires a medical diagnosis.
Symptoms of gluten intolerance generally do not require urgent treatment. They typically resolve with removal of gluten-containing foods within a few days or weeks.
Treatment of gluten intolerance usually includes the complete removal of gluten-containing products from the diet. Some people may also need to take dietary supplements to treat complications.
Untreated non-celiac gluten sensitivity usually does not result in serious complications. Celiac disease, however, could result in complications like anemia, osteoporosis, seizure disorder, infertility, and dental cavities. In children, untreated celiac disease could result in complications like stunted growth, delayed puberty, and failure to thrive.
Save on prescriptions for gluten intolerance with a SingleCare prescription discount card.
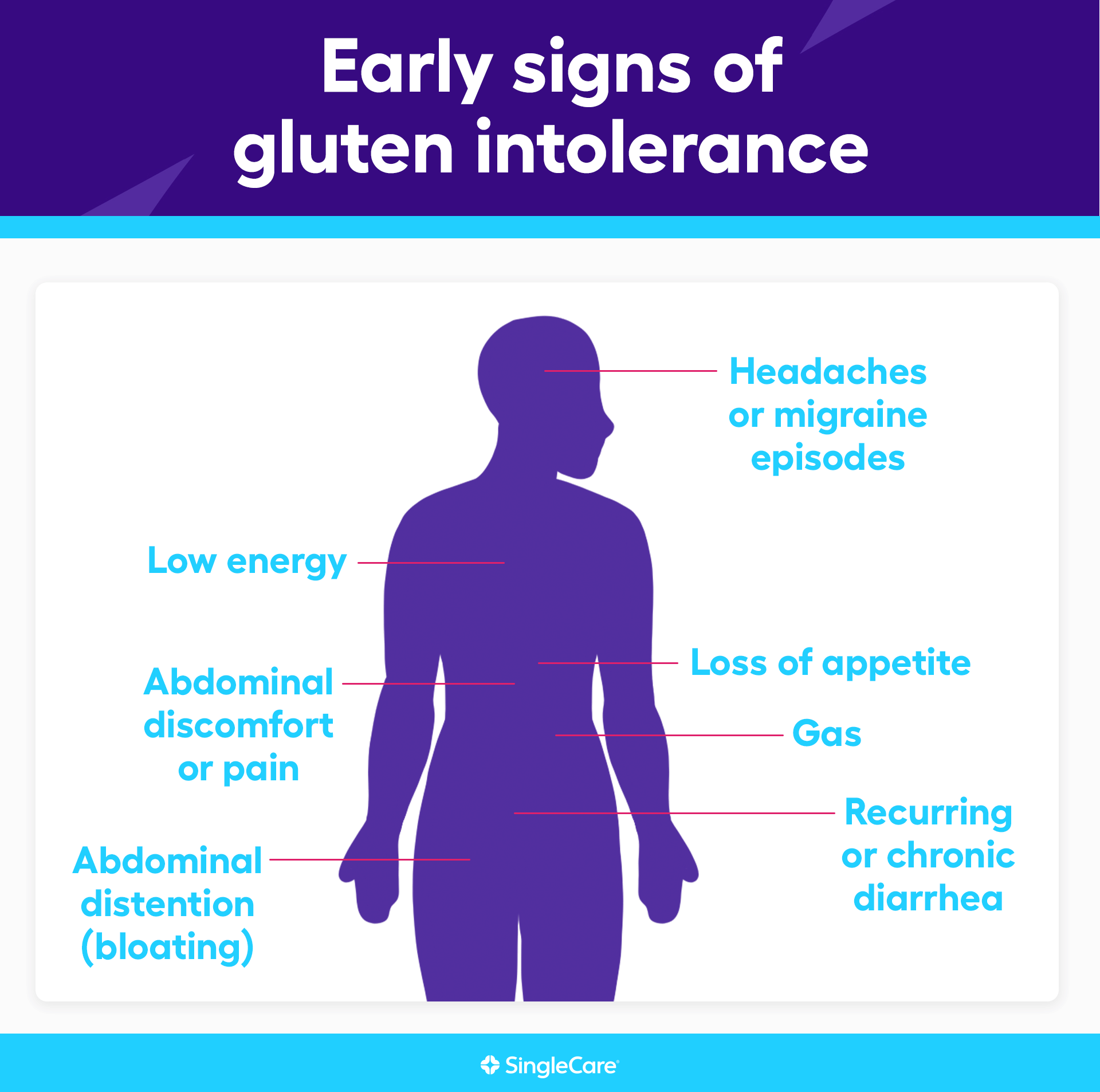
What are the early signs of gluten intolerance?
The earliest and most common symptoms of gluten intolerance are typically digestive system complaints:
Recurring or chronic diarrhea
Abdominal discomfort or pain
Abdominal distention (bloating)
Gas
Loss of appetite
Low energy
Headaches or migraine episodes
Constipation (rare)
For healthcare professionals, chronic or recurring diarrhea may be a warning sign that the problem may be due to gluten intolerance. Oily stools are a sign that the small intestine may not be absorbing nutrients, including fats in our diet.
Other gluten intolerance symptoms
In some cases, celiac disease provokes an immune response in which antibodies not only target a part of the gluten molecule, but also attack the lining of the small intestine. Because the immune system is attacking healthy tissue, celiac disease is considered an autoimmune disease. As the small intestine lining gets damaged, it loses the ability to absorb nutrients. At that point, other parts of the body may begin to show symptoms. These include:
Fatigue
Unexplained weight loss
Vitamin deficiency symptoms such as dizziness, irregular heartbeats, muscle weakness, and shortness of breath
Anemia symptoms such as fatigue, weakness, fast heartbeat , dizziness, and cold hands and feet
Electrolyte deficiency symptoms such as muscle weakness, confusion, brain fog, muscle cramps, and irregular heartbeats
Peripheral neuropathy symptoms such as tingling, numbness, or burning in the hands or feet
Joint pain
Prolonged bleeding or bruising
Balance problems
Depression or anxiety
Irritability
Recurrent blistering skin rash called dermatitis herpetiformis. This can be easily mistaken for eczema or psoriasis
Non-celiac gluten sensitivity vs. celiac disease symptoms
Gluten sensitivity comprises a spectrum of medical conditions. Non-celiac gluten sensitivity is the most commonly reported, affecting roughly 6% of people in the U.S., but the upper end of the range varies based on who’s doing the estimate and which population is being studied. Celiac disease is the most serious form of gluten intolerance and affects 0.5% to 1% of the population. It’s easy to confuse the two. Both have the same digestive system symptoms, and these symptoms are triggered by eating gluten-containing foods. In both cases, symptoms usually clear up when gluten-containing products are removed from the diet. However, celiac disease is a serious medical condition, so it’s important to recognize the differences.
| Non-celiac gluten sensitivity | Celiac disease | |
| Shared symptoms |
|
|
| Unique symptoms |
|
|
Sources:
Gluten-associated medical problems, StatPearls
Celiac Disease, StatPearls
Celiac disease, AMBOSS
Non-celiac gluten sensitivity: a review, Medicina
When to see a doctor for gluten intolerance symptoms
Consult a doctor if gluten intolerance is suspected. Symptoms like chronic or recurrent diarrhea should always be examined by a doctor. It’s important not to self-diagnose gluten intolerance. Though it may only be minor, there is a possibility that it could be something worse.
A doctor will take a medical history and perform a physical exam. However, the condition can not be diagnosed from the symptoms alone. If there are signs of gluten intolerance, the doctor will perform a blood test to measure certain antigens and antibodies. A specialist in digestive system disorders will examine the upper small intestine using endoscopy, a procedure that involves inserting a small camera attached to a long tube into the digestive system. The final diagnosis is made by taking several tissue samples from the small intestine and examining them under a microscope.
If the blood tests and biopsies reveal no evidence of celiac disease, then the doctor will diagnose the problem as non-celiac gluten sensitivity, but only if the symptoms resolve by removing gluten-containing foods from the diet. After a few weeks, the doctor may ask the patient to gradually reintroduce gluten into the diet to see if symptoms return.
Complications of gluten intolerance
Non-celiac gluten sensitivity carries no risk of complications. It is not a true gluten allergy, so severe allergic reactions like anaphylaxis, a life-threatening reaction, are not associated with the condition.
On the other hand, celiac disease can cause complications such as
Vitamin deficiencies
Electrolyte deficiencies
Anemia due to B12, folate, or iron deficiency
Bleeding and bruising
Loss of bone density
Intestinal cancer
Infertility (in women)
Untreatable celiac disease
Neurologic problems such as seizures
Elevated liver enzymes
Pyschiatric problems such as anxiety and depression
For this reason, celiac disease requires greater adherence to treatment and careful monitoring by both the patient and healthcare professionals for any sign of malnutrition or complications.
How to treat gluten intolerance symptoms
The only effective treatment for gluten intolerance (both for non-celiac gluten sensitivity and true celiac disease) is a strict gluten-free diet. Most symptoms will clear up in a few days, but diarrhea and vitamin deficiencies may persist for longer. People who have nutritional deficiencies due to celiac disease may require dietary supplements. Lifetime monitoring in celiac disease is required to ensure adherence to the diet and spot possible complications.
Living with gluten intolerance
The best way to live with gluten intolerance is to strictly avoid foods that contain gluten. Admittedly, that’s hard to do. Avoiding cereals and bread is a logical choice, but most people are unaware of just how many sources of gluten they ingest every day, including prescription drugs. It’s easy to go off a gluten-free diet without even knowing it, so the best advice is:
Always read the list of ingredients for anything you eat
For drugs, read the ingredients list on the package or drug information insert
Keep a list of food ingredients that contain gluten
Most importantly, see a doctor
What you might suspect is that gluten intolerance could actually be a serious problem. The only way to know is to get a medical diagnosis. A healthcare professional can run the tests needed to distinguish a less hazardous sensitivity to gluten from celiac disease and other possible problems like irritable bowel syndrome. The only treatment for gluten intolerance is to eat only gluten-free foods, and this can be very hard to get right. Gluten is present in many different foods, and so seeing a licensed dietitian is also recommended for advice and a proper diet.
FAQs about gluten intolerance symptoms
What does a “gluten belly” look like?
One of the symptoms of gluten intolerance is bloating, or what is popularly known as “gluten belly.” Lower digestive tract bloating is usually caused by food not being properly digested or absorbed. Does “gluten belly” look unique in some way? No, not really. The intestines make up most of the middle and lower abdomen, so “gluten belly” will look like any other type of lower digestive tract bloating. However, if bloating seems to be a regular or constant problem, that’s a possible sign that it may be due to gluten intolerance.
RELATED: Home remedies for bloating
How long after eating gluten do gluten intolerance symptoms start?
There is no agreement on when gluten intolerance symptoms start after eating gluten. It may take hours, days, or weeks. One way doctors diagnose non-celiac gluten sensitivity is to put patients on a gluten-free diet for several weeks, see if symptoms subside, and then gradually reintroduce gluten into the diet to see if symptoms return. They typically allow several weeks on a gluten diet for symptoms to appear.
How long do gluten intolerance symptoms last?
Most gluten intolerance symptoms clear up within a few days after gluten-containing foods are taken out of the diet. Some symptoms may hold on a bit longer, like diarrhea. People with celiac disease may require a few weeks for body-wide symptoms to improve.
What’s next? Additional resources for people with gluten intolerance symptoms
Test and diagnostics
ACG clinical guidelines: diagnosis and management of celiac disease, The American Journal of Gastroenterology
Celiac disease, AMBOSS
Celiac Disease, StatPearls
Gluten-associated medical problems, StatPearls
Non-celiac gluten sensitivity: a review, Medicina
Treatments
ACG clinical guidelines: diagnosis and management of celiac disease, The American Journal of Gastroenterology
Celiac disease, AMBOSS
Celiac Disease, StatPearls
Non-celiac gluten sensitivity: a review, Medicina
Scientific studies and clinical trials
“Brain fog” improves in celiac disease patients after starting a gluten-free diet, Celiac Disease Foundation
Non-celiac gluten sensitivity: how its gut immune activation and potential dietary management differ from celiac disease, Molecular Nutrition & Food Research
Recent advances in understanding non-celiac gluten sensitivity, F1000 Research
More information on related health conditions
IBS treatment and medications, SingleCare
The best IBS diets, SingleCare
Jesse P. Houghton, MD, FACG, was born and raised in New Jersey, becoming the first physician in his entire family. He earned his medical degree from New Jersey Medical School (Now Rutgers Medical School) in 2002. He then went on to complete his residency in Internal Medicine and his fellowship in Gastroenterology at the Robert Wood Johnson University Hospital in 2005 and 2008, respectively. He moved to southern Ohio in 2012 and has been practicing at Southern Ohio Medical Center as the Senior Medical Director of Gastroenterology since that time.
Dr. Houghton is the author of What Your Doctor Doesn't (Have the Time to) Tell You: The Gastrointestinal System. He is also an Adjunct Clinical Associate Professor of Medicine at the Ohio University School of Osteopathic Medicine. He has been in practice since 2008 and has remained board-certified in both Internal Medicine and Gastroenterology for his entire career. He has lent his expertise to dozens of online articles in the medical field.
...Recetas Populares
SingleCare es un servicio de descuentos para medicamentos recetados que ofrece cupones gratuitos para miles de medicamentos. Puedes usarlo aun si tienes seguro, Medicare, Medicaid o no, pero no se puede combinar con el seguro.
SingleCare ofrece transparencia al mostrar los precios de medicamentos para que puedas comparar descuentos en farmacias cerca de ti. Visita singlecare.com para encontrar descuentos en medicamentos, información útil sobre tu receta médica y recursos que te ayudan a tomar decisiones informadas sobre tu salud.
Los ahorros en recetas varían según la receta médica y la farmacia, y pueden alcanzar hasta un 80% de descuento sobre el precio en efectivo. Este es un plan de descuento de recetas médicas. NO es un seguro ni un plan de medicamentos de Medicare. El rango de descuentos para las recetas médicas que se brindan bajo este plan, dependerá de la receta y la farmacia donde se adquiera la receta y puede otorgarse hasta un 80% de descuento sobre el precio en efectivo. Usted es el único responsable de pagar sus recetas en la farmacia autorizada al momento que reciba el servicio, sin embargo, tendrá el derecho a un descuento por parte de la farmacia de acuerdo con el Programa de Tarifas de Descuento que negoció previamente. Towers Administrators LLC (que opera como “SingleCare Administrators”) es la organización autorizada del plan de descuento de recetas médicas ubicada en 4510 Cox Road, Suite 11, Glen Allen, VA 23060. SingleCare Services LLC (“SingleCare”) es la comercializadora del plan de descuento de prescripciones médicas que incluye su sitio web www.singlecare.com. Como información adicional se incluye una lista actualizada de farmacias participantes, así como también asistencia para cualquier problema relacionado con este plan de descuento de prescripciones médicas, comunícate de forma gratuita con el Servicio de Atención al Cliente al 844-234-3057, las 24 horas, los 7 días de la semana (excepto los días festivos). Al utilizar la aplicación o la tarjeta de descuento para recetas médicas de SingleCare acepta todos los Términos y Condiciones, para más información visita: https://www.singlecare.com/es/terminos-y-condiciones. Los nombres, logotipos, marcas y otras marcas comerciales de las farmacias son propiedad exclusiva de sus respectivos dueños.
Los artículos del blog no constituyen asesoramiento médico. Su propósito es brindar información general y no sustituyen el asesoramiento, diagnóstico ni tratamiento médico profesional. Si tiene alguna pregunta sobre una afección médica, consulte siempre a su médico u otro profesional de la salud cualificado. Si cree tener una emergencia médica, llame inmediatamente a su médico o al 911.
© 2026 SingleCare Administrators. Todos los derechos reservados
© 2026 SingleCare Administrators. Todos los derechos reservados







