Diabetes, or diabetes mellitus, is a chronic health condition in which too much sugar remains in the bloodstream. When we eat, our food is broken down into sugar, or glucose, that is released into the bloodstream, triggering the pancreas to produce a hormone called insulin. Normally, insulin acts to help your body turn that glucose into energy. But when your body either doesn’t make enough insulin or it has become insulin resistant, you can develop diabetes, meaning your body cannot effectively process and use sugar.
Although there is no cure for diabetes, lifestyle changes can go a long way in managing the disease and boosting your overall well-being. Along with maintaining a healthy body weight and eating a healthy diet, exercise is one of the most effective ways to keep your diabetes in control.
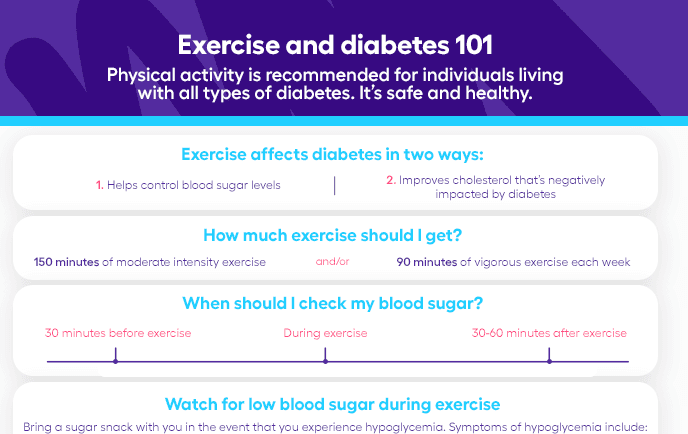
How does exercise affect diabetes?
Exercise can improve symptoms of diabetes in a couple ways by helping your body maintain healthy blood glucose control and cholesterol levels.
Blood sugar
Physical activity increases your body’s sensitivity to insulin, allowing your body to convert blood sugar to energy, according to the Centers for Disease Control and Prevention (CDC). Exercise also serves to control blood sugar levels, thereby decreasing your risk of heart disease as well as the nerve damage that can occur after long periods of elevated blood sugar levels. “If exercise could be bottled and sold [as a] treatment for diabetes, it would have a glucose-lowering effect that lasts for hours,” says Angela Ginn-Meadow, RD.
A regular exercise program is of great importance to our overall health. Benefits include physical strength, balanced mood, weight regulation, and blood glucose control, says Minisha Sood, MD, a board-certified endocrinologist at Lenox Hill Hospital. “Exercise lowers glucose levels and leads to a better insulin response,” Dr. Sood says. There are some exceptions to this, she says, but generally, controlling your weight through lifestyle modifications such as exercise lowers the risk of complications from diabetes. Diabetes complications include:
- Diabetic ketoacidosis (dangerously high levels of ketones in the body)
- Skin complications (bacterial or fungal infections, skin eruptions and rashes)
- Eye complications (cataracts, glaucoma, retinopathy)
- Foot complications (neuropathy, or nerve damage, circulation issues)
- Kidney disease (nephropathy)
- Cardiovascular disease
- High blood pressure
- Stroke
Exercise increases the uptake of blood glucose into the muscle cells, which are the primary disposal site for excess blood sugar, says Barry Sears, Ph.D., a dietary hormone response expert and president of Inflammation Research Foundation. Exercise stimulates muscle cells to increase sugar intake and utilization, thus decreasing blood sugar levels. Sears adds that exercise can decrease diabetes risk as well as make it easier to manage existing diabetes.
Cholesterol
Diabetes tends to lower levels of high density lipoprotein (HDL), the good cholesterol in the body, and raise levels of triglycerides, increasing your risk of heart attack and stroke, states The American Heart Association. Exercise can help you to avoid this.
Exercise helps to improve symptoms of all four types of diabetes, which are:
- Type 1 diabetes patients make up 5%-10% of people with diabetes. It is thought to be caused by an autoimmune reaction in the body that attacks insulin-producing cells (beta cells) in the pancreas. This type of diabetes is not reversible, but can be managed with a combination of healthy lifestyle choices and insulin injections.
- Type 2 diabetes is the most common, making up over 90% of people with diabetes. Type 2 diabetes patients have insulin resistance, meaning their cells don’t respond normally to insulin. As a result, the pancreas goes into overdrive but cannot keep up, and blood sugar levels remain elevated. Obesity is a risk factor, but diabetes can be managed and even reversed with exercise, especially when a healthy, low-cholesterol, low-glycemic diet is adapted (along with weight loss when needed).
- Prediabetes is a chronic health condition in which blood sugar levels are consistently elevated, but not enough to be classified as Type 2 diabetes. A regular exercise routine can help reverse prediabetes.
- Gestational diabetes is a type of diabetes that develops in pregnancy in women. Though blood sugar levels usually go back to normal after the baby is born, up to 50% of women with gestational diabetes will develop Type 2 diabetes. Diet and exercise provide important health benefits that prevent this from occurring.
RELATED: What are carbohydrates?
Is working out with diabetes safe?
Physical activity is recommended for individuals living with all types of diabetes, says Ginn-Meadow, but speak with your doctor for a pre-exercise medical clearance before beginning an exercise program. “This will provide insight into the types of exercise that are best for you, and give you the green light to get started,” Ginn-Meadow says. “If you are living with complications from diabetes, there will be some activities that require modification and/or avoidance. For example, if you have diabetic retinopathy, you may be advised to avoid strength training to prevent further damage.”
For people on insulin, precautions must be taken to lessen the risk of hypoglycemia (low blood glucose), says Dr. Sood. “It’s important for anyone to be well-hydrated prior to exercise but especially for those with diabetes, because dehydration can lead to glucose elevations,” she says. “Aerobic activities like brisk walking, running, bicycling and the elliptical are likely to lower blood glucose levels. Activities such as resistance training and weight lifting or high-intensity interval training (HIIT) may temporarily elevate blood glucose levels, which will then fall over the following 24-48 hours to lower levels.”
If you will be doing performance or competitive exercise, it may be beneficial to work with a sports and fitness dietitian who is also diabetes knowledgeable. Before working out, make sure you eat a balanced meal of complex carbohydrates, proteins, and fats to give you consistent energy.
What’s the best time of day to exercise?
When it comes to diabetes and exercise, the important thing is that you’re doing it, says Ginn-Meadow. “The best time to exercise is the best time for your lifestyle. There is no perfect time; exercise has benefits from two to 48 hours [afterward],” she says. However, to ensure adequate sleep, it is recommended not to exercise for about two hours before you go to bed.
How much exercise should I get?
“The exercise recommendation is 150 minutes of activity per week. So, having 30 minutes of aerobic activity such as walking five days of week would meet the activity target,” Ginn-Meadow explains. The CDC also advises including activities to target all of your major muscle groups (legs, hips, back, abdomen, chest, shoulders, and arms) at least two times per week.
When should I check my blood sugar?
A good rule of thumb when you’re working out with diabetes is to check your blood sugar before, during, and after exercise. If you’re taking a medication such as insulin that is known to cause low blood sugar (hypoglycemia), you should check your blood sugar 30 minutes before exercise, says Dr. Sood, and if you experience symptoms of low blood glucose during exercise, check your blood sugar. It is important to always have a sugar snack with you during exercise in the event that you experience hypoglycemia.
Symptoms of hypoglycemia include weakness, dizziness, tiredness, hunger, shaking, heart palpitations, and changes in mood. “Having a medical ID is important for the prevention and treatment of this emergency,” Dr. Sood recommends. She advises patients to check their blood sugar once again 30-60 minutes post exercise and says that the use of a continuous glucose monitor is very helpful in this regard.
How much exercise is too much for a diabetic?
Your body will let you know if you are doing too much, says Ginn-Meadow. Listen to your body, and if you’re experiencing shortness of breath or muscle pain, slow down and take a break, she says. If you begin to feel any of the symptoms of hypoglycemia, stop exercising. Other important warning signs include headache, fatigue, shakiness, muscle cramping, visual changes, or lightheadedness.
Best exercises for diabetes
The American Diabetes Association (ADA) recommends people with all types of diabetes get a minimum of 150 minutes of moderate intensity exercise and/or 90 minutes of vigorous exercise each week. It’s important to incorporate both aerobic and strength training into your exercise routine, says Sears. Aim for three to five days of aerobic activity and two to three days of resistance exercises, says Ginn-Meadow. Ideally, non-exercise activity would include movement throughout the day and avoidance of prolonged sitting, adds Dr. Sood.
According to research, aerobic exercise like walking improves glucose control, enhances insulin sensitivity, and decreases cardiovascular risk factors of diabetes. Although walking isn’t a cure for diabetes, walking after meals is an effective way to lower blood sugar, Dr. Sood says. Examples of aerobic exercise include:
- Walking
- Using stairs instead of an elevator or escalator
- Swimming
- Biking
- Rowing
- Dancing
- Skating
- Raking leaves or gardening
- Cleaning
Exercise for Type 2 diabetes
Research shows that resistance training is an effective form of exercise for managing glucose homeostasis in Type 2 diabetes. Resistance exercise includes:
- Lifting weights
- Resistance band exercises
- Body weight exercises like lunges and planks
- Balance Training
- Yoga/Tai Chi
- Pilates
Exercise for gestational diabetes
For women with gestational diabetes, walking and yoga are great ways to stay limber, active, and manage blood sugar, recommends Ginn-Meadow. But be sure to consult with a healthcare provider for advice on gestational diabetes management.
“It is recommended that women with gestational diabetes engage in moderate physical activity 20-30 minutes each day,” Dr. Sood says. “This will depend on one’s level of fitness and conditioning prior to pregnancy. If someone was sedentary prior to pregnancy, moderate activity may be brisk walking, [whereas] if someone trained for triathlons, moderate activity would be defined differently.”
Exercises to avoid
There are no specific exercises to avoid with diabetes, but watch out for symptoms such as dizziness, blurry vision, imbalance, confusion, fast heart rate, and shakiness, which may indicate low blood glucose, says Dr. Sood.
Exercise and diabetes medications
A pre-exercise medical clearance can help you better understand the impact of regular exercise on your diabetes, says Ginn-Meadow. “Often diabetes medication doses can be lowered when adding activity,” she says. “Speak with your diabetes care team to create an exercise plan to discuss the time, frequency and intensity of exercise as well monitoring guidelines, snack ideas, medication adjustments and when not to exercise.”
Exercise is safe when on diabetes medications for the most part, says Dr. Sood. “The non-insulin medications like metformin, GLP-1 receptor agonists and SGLT2-inhibitors are less likely to be problematic,” she explains. “There is a group of medicines called sulfonylureas, which cause the body to produce more insulin—these can cause low blood glucose levels and the dose is hard to adjust prior to exercise from day to day,” she says. For people taking insulin, it is important to work with your healthcare provider to plan dosage and scheduling tailored to your exercise program.