A diet low in residue, called the low-residue diet (similar to a low-fiber diet), is often used to manage certain diseases of the gastrointestinal system. It is made up of gut-friendly foods known to reduce digestive symptoms like abdominal pain, diarrhea, constipation, and altered bowel habits. The low-residue diet is part of the therapy for those with short gut syndrome, certain patients with irritable bowel syndrome (IBS), acute diverticulitis, gastroparesis (slow stomach emptying) and bowel narrowing or obstruction. It is also a diagnostic diet recommended before colonoscopy.
What is a low-residue diet?
A low-residue diet is an eating plan that limits or eliminates certain foods known to trigger gastrointestinal distress. “It is usually recommended when there is an inflammatory or obstructive process in the colon or small intestine that would impede the passage of more fibrous nutrients, risking a bowel obstruction,” says Joseph D. Pianka, MD, a board-certified gastroenterologist in Rhode Island. Consequently, the diet emphasizes easy-to-digest foods while restricting indigestible food materials—because they increase the volume and amount of stool produced by the digestive tract.
Additionally, a low-residue diet aims to reduce the food waste that builds up in your large intestine to form “residues.” A residue comprises undigested foods, gut microorganisms, and other intestinal secretions that remain after digestion and contribute to the bulk of your poop.
The low-residue diet is a therapeutic diet designed to help people with gastrointestinal conditions—such as ulcerative colitis and Crohn’s disease (together termed inflammatory bowel disease), bowel inflammation, diverticulitis, and irritable bowel syndrome (IBS)—and patients who cannot tolerate foods high in fiber. It helps to limit bowel movement, frequency of defecation, and overall stool bulk. A gastroenterologist may recommend a low-residue diet before a colonoscopy or colorectal surgery for bowel preparation (cleansing the intestine of fecal materials) and post-operation to hasten a patient’s recovery.
RELATED: IBD vs. IBS
How does the low-residue diet work?
When digestive issues flare up, consuming low-residue foods may be necessary to provide symptomatic relief. Typically, the low-residue diet works by eliminating foods believed to produce high amounts of residues/undigested fiber that trigger gastrointestinal flare-ups.
For example, foods such as fruits, vegetables, and whole grains are restricted because of the fiber content, as fiber produces high amounts of residues. A study published in the World Journal of Gastroenterology showed that reducing fiber intake improved conditions of people with chronic constipation. Fiber increases the bulk of feces, so eliminating high-fiber foods from their diet relieved the patients by reducing the size and volume of stool—so the patients could pass smaller, thinner stools. It should be noted, however, that many gastroenterologists recommend starting treatment with a high-fiber diet in patients with constipation.
This is why a low-residue diet consists of predominantly low-fiber foods. A maximum of 10 g of fiber per day is the recommended intake for this diet, which stands in contrast to the dietary fiber recommendation of 30-35 g per day for men and 25-32 g per day for women.
Unlike a strictly low-fiber diet that only restricts fiber intake, a low-residue diet limits fiber and dairy. (Milk and its products also contribute to the buildup of residue.)
“The diet is usually implemented for less than a week, depending on the clinical situation,” Dr. Pianka says. “A good rule of thumb is to continue the diet until symptoms improve, and then gradually add fiber content as tolerated.”
However, the duration can be longer for certain conditions. “Low-fiber diets may be long-term diet plans in those that suffer from chronic illnesses that do not allow them to tolerate daily dietary fiber intake,” says Michelle Pearlman, MD, a gastroenterologist based in Fort Lauderdale, Florida.
According to Ronen Arai, MD, a gastroenterologist with Gastro Health, the diet could also be used long-term in people who have a small intestinal narrowing or chronic narrowing of the bowels.
However, you should only follow a low-residue diet under the supervision of your healthcare provider. This is important because it is an elimination diet—and you may be at risk of nutritional deficiencies.
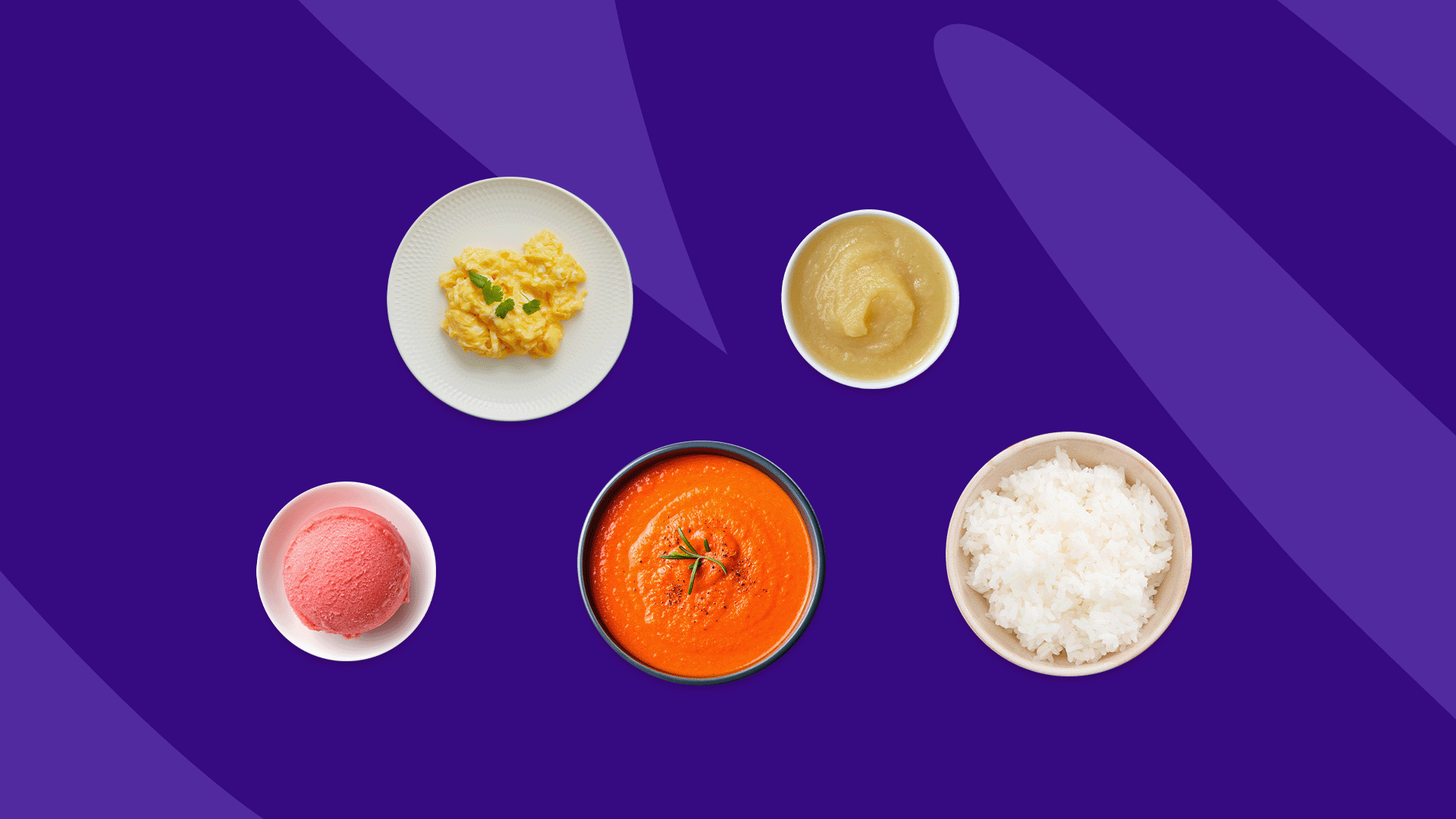
What can I eat on a low-residue diet?
Aim for a balanced diet, but remember that individual food choices differ, and some foods may still upset your system. For this reason, when on a low-residue diet, you need extra care with what you eat.
“Other options to follow a less restrictive diet but still consume nutrient dense foods is to make ‘baby food’ that is often better tolerated,” Dr. Pearlman says. “Steam veggies without the skins and blend, make a puree, eat nut butters instead of whole nuts. Mash beans very well, and consume small amounts of hummus instead of the whole chickpeas. Remove skins from fruit and cook the fruit down well.” Here are some recommended low-residue diet foods you can try.
Breads and cereals
- White bread, refined breads, muffins, quick breads, rolls, and pancakes
- Rice cereal, white rice
- Refined cold cereals such as puffed rice, puffed wheat, cornflakes
- Refined cooked cereals including grits or cream of wheat
- Refined pasta, macaroni, and noodles
Vegetables
- Blended or pureed vegetable soups
- Plain tomato sauce and paste
- Cooked and peeled carrots, pumpkin, turnips, and onion
- Well-cooked broccoli and cauliflower without stalks
- Potato without skin
- Canned vegetables without seeds like green beans, carrots, asparagus (without tips), or diced tomatoes
Meat, fish, and eggs
- Fish without bones
- Boiled, scrambled or poached eggs
- Tender lamb, beef, pork, chicken, turkey, offal (liver, kidney)
- Beef burgers
- Tofu
Fruit
- Peeled and well-cooked fruits like apple, mangoes, and plums
- Seedless peeled grapes, pears, ripe banana, and cantaloupes
- Pureed and sieved fruit juices or fruit juice without pulp
- Applesauce
Fats and oils, sauces, condiments
- Vegetable oils, margarine, and butte
- Soy sauce
- Ketchup
- Creamy peanut butter
Desserts and sweets
- Plain hard candy, and sherbet
- Plain cake, and cookies
- Chocolate without nuts, vanilla waffles
- Frozen pops, gelatin, and custard
- Sugar, honey, jelly, molasses, and syrup
You should also be sure to consume lots of water and decaffeinated tea or coffee to stay hydrated.
What foods should I avoid on a low-residue diet?
You should avoid the following foods if you are on a low-residue diet:
- Soups with chunks of vegetables
- Oranges and other citrus fruits, all berries, raw fruits with membranes, dried fruits like apricots, prunes, and figs
- Fatty meat and gristle
- Lentils, dried beans, peas, and legumes
- All dairy products
- Any whole-grain bread and cereal made with whole grain flour, cornbread, or corn muffins
- High-fiber cereals like porridge oats, bran flakes or granola
- Brown rice
- Most raw vegetables including lettuce, Brussels sprouts, beets, raw onions, cucumber, and raw spinach
- Nuts, coconut, pickles, seeds, and horseradish
- Seasonings and spice like chili powder, cloves, garlic, and pepper
Possible risks of a low-residue diet
Dietary fiber is an essential component of every healthy diet. Consuming adequate fiber in one’s diet has been positively linked to reducing chronic diseases like heart diseases, stroke, obesity, and Type 2 diabetes. Invariably, because a low-residue diet limits dietary fiber intake, it may cause unintended side effects in people who follow it for a long time because of possible nutritional deficiencies.
“There is little to no short-term risk,” Dr. Pianka says. “But long-term, this is usually a high calorie and relatively poor macronutrient selection diet, [so you are] risking weight gain, nutrient deficiencies, and slower transit of digestive waste.”
Moreover, several studies suggest that a low-fiber diet high in refined foods contributes to constipation and can also cause the development of hemorrhoids and diverticulitis. Some other lifestyle changes that may help gastrointestinal symptoms in addition to a low-residue diet include the following.
Relaxation exercises
A pilot study highlighted the benefits of digestion-focused meditation in improving quality of life and gut health and providing symptomatic relief for people with gastrointestinal disorders like irritable bowel syndrome.
According to a Harvard report, relaxation exercises such as meditation and yoga effectively help manage gastrointestinal distress for patients with IBS or IBD. The study reports a notable improvement in patients’ symptoms, anxiety, and overall quality of life. The researchers believe that the mind-body interaction (due to the effect of the relaxation exercises) reduced the impact of the genes known to produce inflammatory responses. They also found that the relaxation exercises made it easier for the participants to effectively endure the pain associated with their condition.
Thus, consider incorporating simple relaxation exercises like yoga and meditation in your daily life to cope, manage your symptoms, and reduce stress and anxiety.
RELATED: The link between physical and mental health
Home remedies
As a general rule it’s a good idea to use the following practices to keep things running smoothly in your digestive system.
- Ensure you stay hydrated and drink plenty of water. Studies have found that dehydration is a common cause of abdominal pain. If abdominal pain is due to dehydration, your healthcare provider may recommend oral rehydration meds such as Pedialyte.
- Cook your foods until they’re tender. Bake, simmer, poach, boil, or steam foods rather than frying and grilling them.
- Besides avoiding hard-to-digest foods, eat mindfully. This means taking small bites, chewing slowly and thoroughly, and stopping eating when you’re full.
- It’s a good idea to get some exercise. Regular physical activity can also benefit gut health.
Medication
Medication can help reduce the severity and frequency of abdominal discomfort. Your healthcare provider may prescribe medications based on a description of your symptoms and how uncomfortable they make you.
For example, prescription meds like rifaximin, eluxadoline, and lotronex are FDA-approved for treating irritable bowel syndrome with diarrhea (IBS-D). However, the prescription may vary depending on the type of condition you have.
Supplements
Fruits, vegetables, and milk—all of which are restricted in a low-residue diet provide an abundance of nutrients such as vitamins A, C, and E, magnesium, zinc, calcium, potassium, and folate. If you are on a low-residue diet, you may benefit from dietary supplements to treat any nutritional deficiencies you may develop because of your diet. If you decide to try supplements, talk to your provider to find out how much and which vitamins & minerals you need.
When to see a doctor
If you have unexplained or persistent abdominal pain or if it hinders your daily life, speak with your healthcare provider. You may want to see a gastroenterologist if these symptoms accompany the abdominal pain:
- Bloody stool or black stool
- Continuing or worsening symptoms of diarrhea, vomiting, and constipation
- Acute or chronic severe abdominal pain (cramps)
- Fecal incontinence
- Heartburn
- Weight loss
- Rectal bleeding
- Fevers or chills
These could be signs of a more serious condition or medical emergency.