Prednisolone is a widely-used prescription drug that treats a wide range of medical conditions. Called a corticosteroid or glucocorticoid, prednisolone pills reduce inflammation, block the immune system, fight leukemia or lymphoma, or can be used to replace cortisol, the body’s natural corticosteroid hormone. Similar to prednisolone, prednisolone sodium phosphate or prednisolone acetate may be prescribed as eye drops to treat eye swelling.
As with all corticosteroids, prednisolone commonly causes side effects. Some can be severe and even life-threatening. Side effects can sometimes be made worse when other drugs are taken. Prednisolone can also worsen pre-existing medical conditions. A little understanding of how prednisolone works as well as a few tips can help minimize problems when taking prednisolone.
RELATED: Learn more about prednisolone
Common side effects of prednisolone
Most people will experience side effects when given prednisolone. Corticosteroids are powerful hormones and affect nearly every major system in the body. Many common side effects are dose-dependent, so higher doses are more likely to cause side effects. The most common side effects of prednisolone are:
Skin problems
- Skin rash
- Hives
- Acne
- Facial redness
- Thinning skin (when taken long-term)
- Skin discoloration
- Skin spots
- Unwanted hair growth
- Excessive sweating
- Slow wound healing (when taken long-term)
Mental and mood changes
- Mood swings
- Anxiety
- Depression
Nervous system problems
- Problems with falling asleep or staying asleep
- Headache
- Dizziness
- Vertigo
- Tiredness
Digestive system problems
- Appetite changes
- Weight gain
- Nausea
- Vomiting
- Heartburn
Fluid and electrolyte problems
- Fluid retention (edema)
- Sodium retention
- Potassium loss
- High blood pressure
Endocrine (hormone) disorders
- Decreased glucose tolerance
- Menstrual irregularities
- Redistribution of body fat (called Cushingoid appearance: puffy face, obese torso, and buffalo hump)
Muscle problems
- Muscle weakness
- Loss of muscle mass
Common side effects of prednisolone eye drops
The most common side effects of prednisolone eye drops are:
- Eye irritation, itching, or burning
- Increased fluid pressure in the eye
- Pupil dilation
- Blurred vision
- Foreign body sensation
- Drooping eyelid
- Taste changes
- Headache
- Rash
- Allergic reactions
Serious side effects of prednisolone
Serious side effects of prednisolone are often dose-dependent and many are primarily due to long-term use.
Mental and mood changes
- Steroid psychosis
Nervous system problems
- Seizures
- Elevated fluid pressure in the brain
Digestive system problems
- Stomach ulcers
- Perforation
- Swelling of the pancreas
Fluid and electrolyte problems
- Hypertension
- Dangerously low potassium levels
- Congestive heart failure
Endocrine (hormone) disorders
- Adrenal insufficiency
- Cushing syndrome
- Diabetes
- Growth suppression in children (when used long-term)
- Withdrawal symptoms if stopped abruptly
Muscle and bone problems
- Muscle damage
- Tendon rupture
- Bone tissue death
- Osteoporosis (when used long-term)
Immune system problems
- Immune suppression (when used long-term)
- Infection
- Kaposi’s sarcoma (when used long-term)
Eye problems
- Glaucoma (when used long-term)
- Cataracts (when used long-term)
- Protruding eyeballs
Severe allergic reactions
- Difficulty breathing
- Anaphylaxis
If you are taking prednisolone and experience symptoms of an allergic reaction such as hives, difficulty breathing, or swelling around the lips, tongue, or face, get emergency medical help right away.
Serious side effects of prednisolone eye drops
When instilled into the eyes, the most serious side effects of prednisolone acetate or prednisolone sodium phosphate eye drops are:
- Eye swelling
- Thinning of the cornea
- Thinning of the whites of the eye
- Corneal sores
- Perforation
- Delayed eye wound healing
- Optic nerve damage
- Eye infection
- Elevated fluid pressure in the eye
How long do prednisolone side effects last?
Many common side effects of prednisolone will rapidly resolve once the drug is stopped. Fluid retention, swelling, mood changes, rash, redness, elevated blood pressure, abdominal discomfort, and irregular menstrual periods are rapidly reversed. Weight gain during a short course of prednisolone is mostly due to fluid retention, so it’s reversed relatively quickly once the drug is no longer taken. However, weight loss after several weeks or months of prednisolone treatment will take diet and exercise to fix.
Other side effects may take longer to resolve such as infections, acne, muscle damage, or tendon damage. Adrenal insufficiency due to high doses or long-term use of prednisolone can take months to return to normal. Withdrawal is a less severe form of adrenal insufficiency and usually takes only a few weeks for symptoms to clear (but may take longer). Some severe side effects, such as diabetes, cataracts, or osteoporosis, can turn into chronic or life-long conditions.
For people taking prednisolone eye drops, irritation, burning, and blurred vision usually only last a few minutes. Other side effects such as vision problems, dilated pupils, and drooping eyelids get better within a few days of stopping the medicine. Some conditions such as vision loss, cataracts, or glaucoma could become lifelong medical conditions.
Prednisolone contraindications & warnings
Prednisolone is a powerful medication that affects nearly every system in the body. Not everyone can take prednisolone without special care.
Abuse and dependence
Prednisolone is not a controlled substance. It is not commonly abused, but it can cause physical dependence and withdrawal by reducing the body’s ability to produce cortisol.
Overdose
The standard prednisolone dose ranges from 5 to 60 mg daily, but some conditions are treated with much higher doses. Unfortunately, the effects of a significantly large overdose taken over a short period have not been studied. Because side effects are dose-dependent, any excessive amount of prednisolone can be expected to increase the likelihood and severity of side effects. If there’s any reason to believe that too much prednisolone has been taken, call a poison helpline and seek emergency medical aid.
Restrictions
Prednisolone may cause problems in people with certain pre-existing medical conditions. For some people, prednisolone can never be given if they have:
- Hypersensitivity to prednisolone
- A fungal infection of the body’s organs
- Cerebral malaria
Although other people with pre-existing conditions can take prednisolone, doses may need adjusting or they may need to be monitored for problems.
- Because prednisolone weakens the immune system, people who are immune-suppressed or who have active infections, tuberculosis, exposure to measles or chickenpox, or any increased risk of infection, will have to be closely monitored for infections when taking prednisolone.
- People with an active herpes zoster infection of the eye should not use prednisolone due to an increased risk of corneal perforation.
- Prednisolone can cause ulcers and perforation, so people with peptic ulcers, diverticulitis, ulcerative colitis, intestinal surgery, or any other risk of perforation will be prescribed prednisolone cautiously and monitored for gastrointestinal problems.
- Side effects are enhanced in people with cirrhosis and hypothyroidism, so dosing may need to be adjusted.
- Pregnant women should talk with a healthcare professional before taking the drug. Healthcare providers prescribe prednisolone cautiously during the first trimester of pregnancy.
- Nursing women will also need to talk with a healthcare provider. Oral corticosteroids do pass into breast milk and could affect an infant’s hormone balance and growth.
- Prednisolone is used cautiously in children and adolescents. Long-term prednisolone treatment could stunt a child’s growth.
- Other medical conditions that will require extra care and monitoring during prednisolone treatment include:
- High blood pressure
- Mental illness
- Diabetes
- Heart problems
- Myasthenia gravis
- Multiple sclerosis
- Kidney problems
- Seizure disorder
- Adrenal gland tumor
- Swelling of the optic nerve
Prednisolone interactions
Taking prednisolone with other prescription or over-the-counter drugs can worsen side effects or cause other health problems.
First, because prednisolone suppresses the immune system, no one receiving prednisolone can be given a live vaccine or Imlygic (talimogene laherparepvec), a live virus used to treat skin cancer. When taking prednisolone, these vaccines could erupt into an active infection.
Prednisolone also should not be taken with mifepristone or desmopressin.
Other drugs may require caution or monitoring when combined with prednisolone. These include:
- NSAIDs: Combining prednisolone with nonsteroidal anti-inflammatory drugs (NSAIDs)—such as aspirin or ibuprofen—or salicylates raises the risk of severe gastrointestinal side effects including perforation.
- Immune–suppressing drugs: Immunosuppressants taken with prednisolone—a drug that also suppresses the immune system—can leave patients dangerously vulnerable to infections and cancer.
- Allergy skin tests: Because prednisolone suppresses the immune system, allergy skin tests are less reliable.
- Vaccines: Live vaccines should not be administered when taking immunosuppressive doses of prednisolone. Inactivated vaccines may be given, but the response cannot be predicted.
- Loop and thiazide diuretics: Because of the risk of potassium depletion, prednisolone is used cautiously with diuretics that do not spare potassium. Other drugs that deplete potassium, such as macrolide antibiotics (like clarithromycin), will also be used cautiously. People taking these combinations may need regular blood tests to monitor potassium levels.
- Quinolone antibiotics: Combining prednisolone with quinolone antibiotics such as ciprofloxacin or moxifloxacin increases the risk of tendon rupture.
- Migraine medications and stimulants: Triptans, ergot drugs, amphetamines, stimulants, and some allergy drugs can add to elevated blood pressure caused by prednisolone.
- Androgens: Testosterone and similar drugs raise the risk of fluid retention and high blood pressure when combined with prednisolone.
- Estrogens: Estrogens may increase the effects of prednisolone.
- Diabetes drugs: Prednisolone may interfere with the ability of diabetes drugs to control high blood sugar.
- Antihypertensives: Prednisolone may interfere with the effectiveness of drugs given to reduce blood pressure.
How to avoid prednisolone side effects
For most people, prednisolone will cause unwanted side effects. There are, however, a few tips that can help minimize or manage these problems.
1. Take prednisolone as directed
Take the dose as prescribed, usually 5–60 mg per day. Prednisolone is usually scheduled to be taken at a particular time of day, so try to take the dose at the correct time.
2. Tell the doctor about all medical conditions and medications
To avoid side effects, tell the doctor or other healthcare provider giving you prednisolone about all your medical conditions, particularly:
- Herpes infection of the eye
- Fungal infection
- Stomach ulcers, diverticulitis, or ulcerative colitis
- High blood pressure
- Mental illness or psychosis
- Liver problems
- Thyroid problems
- Diabetes
- Osteoporosis
- Multiple sclerosis
- Myasthenia gravis
- Pregnancy or pregnancy plans
- Breastfeeding or any plans to breastfeed
Certain drug interactions can cause problems, so make sure the doctor or other healthcare provider knows about all prescription drugs, over-the-counter drugs, and supplements that are taken regularly. When seeing any other healthcare or provider, tell them you are taking prednisolone.
3. Take prednisolone with food
To avoid stomach upset, nausea, and vomiting, take prednisolone with food or milk.
4. Avoid NSAIDs and alcohol
Nonsteroidal anti-inflammatory drugs (NSAIDs) such as aspirin and ibuprofen make the digestive system more likely to be hurt by stomach acid. So avoid them when taking any corticosteroid.
5. Eat a healthy diet
To avoid weight gain, eat a healthy diet when taking prednisolone. Lean protein can satisfy the increased appetite without causing weight gain. Reducing salt intake to less than 2,000 mg a day can help prevent weight gain, fluid retention, and sodium retention. Eat potassium-rich foods to help prevent potassium loss. A nutritionist can help design a prednisolone-friendly diet.
6. Exercise moderately
Another way to avoid weight gain and even promote weight loss is to exercise moderately. The key is to take it easy. Prednisolone can affect muscle strength, muscle mass, connective tissues, and bone density, especially when taken long-term. Ask your doctor about an appropriate and safe exercise regimen.
7. Take calcium and vitamin D supplements
Prednisolone disrupts the body’s ability to regulate calcium and, as a result, leeches calcium from the bones. To help reduce bone loss, take calcium and vitamin D supplements when taking prednisolone. Your healthcare professional can advise you on the appropriate dose.
8. Avoid infections
The body is less able to fight off infections during prednisolone treatment. Avoid people who are sick. Wash your hands regularly. Get medical advice if you notice signs of infection such as high fever or pain during urination.
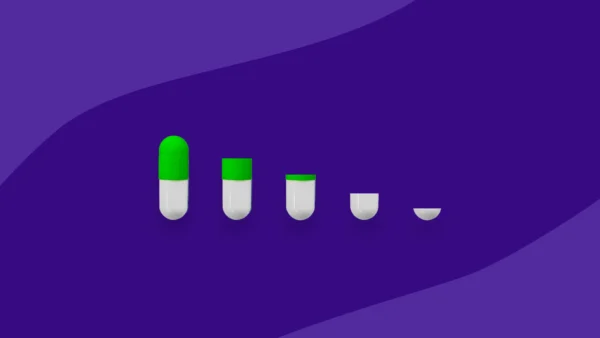
9. Do not stop taking prednisolone without consulting your doctor
Prednisolone can cause withdrawal symptoms when stopped suddenly. These symptoms could last for weeks or even months depending on the dose and duration of prednisolone treatment. The best way to stop taking prednisolone—even for short-term treatment—is a tapered dose prescribed by a doctor or other healthcare professional.
Resources:
- Corticosteroid-induced bradycardia, Canadian Pharmacists Journal
- Episodes of shortness of breath induced by prednisone, The Netherlands Journal of Medicine
- FAQ: Prednisone, UCSF Health
- Guidelines for a low sodium diet, UCSF Health
- Prednisolone, Epocrates
- Prednisolone acetate, Epocrates
- Prednisolone sodium phosphate oral solution prescribing information, U.S. National Library of Medicine
- Prednisolone syrup drug summary, Prescriber’s Digital Reference