Key takeaways
Most insurance providers do not cover GLP-1 medications like Ozempic for the treatment of PCOS, as it is not currently FDA-approved for such use.
You may be able to receive insurance coverage if your PCOS co-occurs with another diagnosis, such as Type 2 diabetes, or if your healthcare provider can provide documentation proving the need for Ozempic to manage symptoms.
If your request for coverage is denied, you may be able to file an appeal, consider alternative treatments, or use a coupon as an alternative.
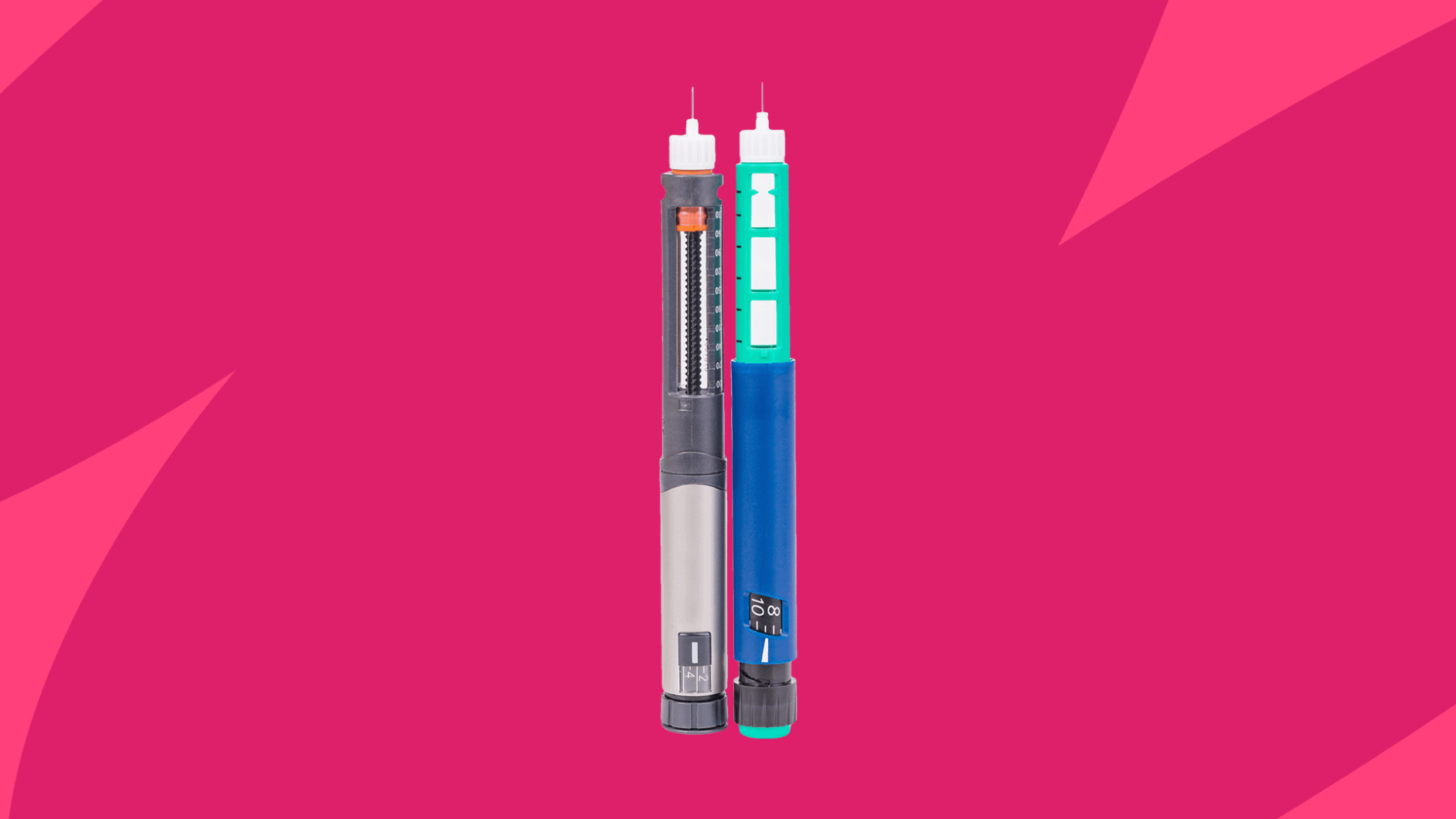
Ozempic (semaglutide), a GLP-1 receptor agonist, is a prescription medication most commonly used to manage blood sugar levels in people with Type 2 diabetes. It may also be prescribed off-label for weight loss, weight management, or polycystic ovary syndrome (PCOS) to help regain insulin sensitivity and reduce symptoms. However, Ozempic is not approved by the U.S. Food and Drug Administration (FDA) to treat PCOS—it is solely approved to manage Type 2 diabetes.
Is Ozempic covered for PCOS?
So, will insurance cover Ozempic for polycystic ovarian syndrome? Unfortunately, most health insurance companies will not cover Ozempic for PCOS, as the injectable drug is not FDA-approved to treat the reproductive health condition. It’s only approved to manage blood sugar levels, prevent cardiovascular events, and prevent kidney disease in people with Type 2 diabetes.
In certain scenarios, coverage may be more likely, depending on a person’s prior medical history or current health conditions. For example, if PCOS co-occurs with prediabetes or diabetes, you may be able to get your insurance to cover Ozempic and reap the benefits for your PCOS, too.
PCOS symptoms may include:
- Irregular periods, extremely difficult menstrual cycles, or bleeding without ovulation
- Fertility issues
- Pelvic pain
- Weight gain, difficulty losing weight, or other metabolic issues
- Obesity
- Hirsutism (excessive hair growth)
- Acanthosis nigricans (darkened skin)
- Oily skin
- Acne
In addition, people diagnosed with obesity who have not responded to lifestyle changes targeting weight management or other weight loss medications may be able to get Ozempic covered by their insurance. “If a patient has a BMI over 30, or over 27 with at least one weight-related health condition, some insurers will approve coverage after a prior authorization process that documents the medical necessity and failed attempts with other therapies,” says Dr. Suzanne Manzi, MD, a board-certified obesity medicine, pain medicine, rehabilitation, and electrodiagnostic medicine physician and co-founder of Performance Pain and Sports Medicine in Houston, Texas. “I have had patients get Ozempic covered if they meet criteria for obesity (with or without PCOS), or if they have prediabetes in addition to PCOS.”
How to get Ozempic covered for PCOS
With your healthcare provider‘s help, it’s possible to get Ozempic covered by your insurance for the treatment of PCOS. However, a few things may need to be done before you get a prescription.
Here are a few common strategies for getting insurance coverage for Ozempic to treat polycystic ovarian syndrome:
Get a strong diagnosis with documentation
Dr. David Ghozland, MD, a board-certified obstetrician and gynecologist in Orange, California, says that documentation is crucial when dealing with an insurance provider. “To gain approval, one has to develop good documentation,” he explains. “I order full metabolic panels, such as fasting insulin, that can indicate resistance in the case of glucose that seems normal. Then, I order metformin, record four months of inadequate response or unacceptable adverse effects, and write an elaborate letter to put this in the framework of insulin resistance treatment and not the management of PCOS.”
Dr. Ghozland shares that the more evidence you can provide to your insurance provider, the better. “My best way to go is to add photos of acanthosis nigricans or laboratory confirmation of high androgen levels since a visual representation cannot be ignored,” he says. “The insurers react to the information that they cannot refute, and that is why you need to create an airtight medical history that would bind all the symptoms to metabolic dysfunction that the given drug is needed to address.”
Emphasize co-occurring conditions
While some PCOS symptoms, such as excess hair growth, darkened skin, and acne, are not serious, PCOS can also occur alongside more serious health issues.
Dr. Manzi explains that highlighting health risks and comorbidities, such as prediabetes, metabolic syndrome, hypertension, or other cardiovascular issues like heart disease or impaired glucose tolerance, can strengthen the case for medical necessity. “Many insurers look for these risk factors when considering coverage,” she adds.
Request prior authorization
If your healthcare provider has considered all treatment options and strongly believes that Ozempic is the best choice for your PCOS, they can submit a prior authorization (PA) request to your insurance provider. This is when your healthcare provider contacts your insurance company to explain why a medication or treatment is medically necessary and to request coverage on your behalf.
“I usually submit a detailed PA letter that outlines failed therapies, severity of symptoms, and the evidence behind Ozempic’s use in PCOS with obesity or metabolic dysfunction,” Dr. Manzi says. “Attaching research summaries or guideline statements (such as those from StatPearls or the American Association of Clinical Endocrinology) sometimes makes the difference.”
Ozempic cost without coverage
Without insurance coverage, Ozempic can be expensive. One 2 mg/3 mL multi-dose prefilled pen (0.25 mg or 0.5 mg/dose) costs about $1,393 without insurance. At a dosage of 0.5 mg per week, Ozempic can cost nearly $16,716 each year if you’re uninsured.
Pricing may vary depending on your dosage and the pharmacy you choose. Having insurance or other financial support could significantly lower your out-of-pocket costs.
What to do if your health insurance doesn’t cover Ozempic
Having your health insurance provider deny coverage for a potentially helpful medication can be discouraging, but it doesn’t mean that you’re out of options.
Here are a few ways to find treatment that fits your budget:
Use a SingleCare coupon
If you’re prescribed Ozempic off-label for symptoms of PCOS, there are ways to make it more affordable—even without health insurance. A SingleCare discount card can help you get access to Ozempic or other semaglutide treatments at a lower cost. With this savings card, you could pay as low as $844 for one Ozempic 2 mg/3 mL prefilled multi-dose pen (0.25mg or 0.5mg/dose).
This discount card can be used in place of insurance and may sometimes be more cost-effective than a copay. Some people save up to 80% off their prescription drug prices. The SingleCare prescription savings card is accepted at several major U.S. pharmacies.
To get the free SingleCare discount card, search for your preferred pharmacy on the Ozempic page of the SingleCare website. From there, you’ll be prompted to click “Get free coupon,” which will share a coupon you can save to your phone or print. Simply present the coupon to your pharmacy to receive a discount on your semaglutide injections.
Save up to 80% on Ozempic with SingleCare
Different pharmacies offer different prices for the same medication. SingleCare helps find the best price for you.
File an appeal
Insurance companies have specific appeal processes that healthcare providers can follow to demonstrate that a person needs a specific medication. “Some patients have succeeded after their specialist or primary care provider appeals a denial with supporting documentation, or after switching to a plan with better obesity medication coverage,” Dr. Manzi says.
If your coverage request is initially denied, talk to a healthcare provider about filing an appeal that highlights why you should qualify.
Consider alternative treatments
While the FDA may not yet approve Ozempic to treat PCOS, there are other options you can explore that may be covered by your insurance plan.
The FDA acknowledges that there’s no one-size-fits-all approach to treating PCOS—there are several approaches that can help relieve symptoms.
These include:
- Oral contraceptives: May help manage or regulate menstrual cycles.
- Medications: Metformin or Mounjaro (tirzepatide) may help with insulin resistance.
- Lifestyle changes: A low-carb diet and regular exercise can help lower blood sugar and support weight loss. People with PCOS often begin seeing symptom improvement with a significant weight loss of over 5% of their total body weight.
- Hair removal: Oral medication (such as spironolactone), electrolysis, or laser treatment can help remove unwanted hair caused by excess androgens.
- Surgery: In some cases, surgical treatment may be recommended if a person is not responding to medication. However, this is often a last resort, as other treatments are typically effective.
- An update on contraception in polycystic ovary syndrome, Endocrinology and Metabolism (2021)
- Polycystic ovary syndrome (PCOS) blog, U.S. Food & Drug Administration (2024)
- PCOS and unwanted facial hair, PCOS Awareness Association
- Is there still a place for surgery in patients with PCOS? A review, Life (Basel) (2023)
- Dr. Suzanna Manzi, MD of Performance Pain and Sports Medicine
- Dr. David Ghozland, MD of David Ghozland, MD