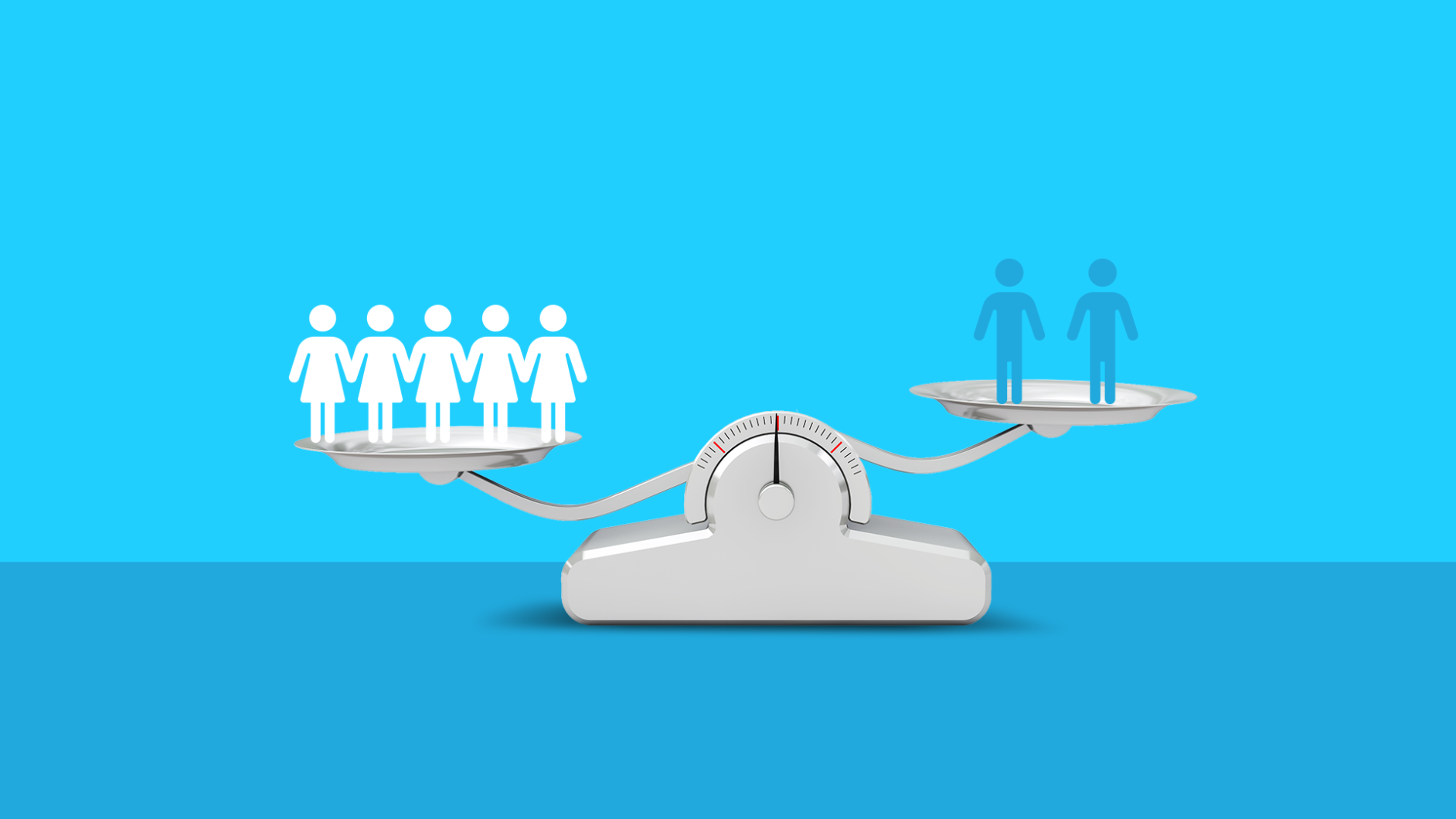
When I was diagnosed with rheumatoid arthritis, I immediately wanted to know more about the disease and how it would likely impact my quality of life. One fact I was surprised to discover is that while around 8% of the population is affected by autoimmune disease, women make up close to 80% of all cases in the U.S. Why are women so disproportionately affected? To find answers, it’s important to first understand what constitutes an autoimmune disorder.
What are autoimmune disorders?
An autoimmune disease occurs when the immune system, which normally fights off viruses, bacteria, and infection mistakenly attacks your body. There are more than 100 autoimmune diseases. Each disease is unique, but many share these symptoms:
- Fatigue
- Dizziness
- Difficulty concentrating
- Low-grade fever
- Numbness and tingling in the hands and feet
- Hair loss
- Skin changes or rashes
Because these initial symptoms are somewhat vague, it can be difficult (and take some time) to get the correct diagnosis. Autoimmune diseases are typically diagnosed through a comprehensive history and physical examination, blood tests, imaging (X-rays, MRI’s, and ultrasound tests), and other diagnostics.
What are the most common autoimmune diseases?
Some of the most common autoimmune diseases include:
- Thyroid diseases
- Psoriasis
- Type 1 diabetes
- Inflammatory bowel disease
- Rheumatoid arthritis
- Lupus
- Multiple sclerosis
Women tend to develop autoimmune diseases during their childbearing years, between ages 12 and 51. “Autoimmune diseases like rheumatoid arthritis, lupus, Hashimoto’s disease [low thyroidism], Sjogren’s syndrome, Grave’s disease [high thyroidism], and multiple sclerosis affect women more than men,” says Magdalena Cadet, MD, a New York–based rheumatologist and associate attending at NYU Langone Medical Center.
Why do women have more autoimmune diseases than men?
Most experts believe it’s a combination of hormones (primarily estrogen), genetics (the X chromosome), and immune system response.
Evidence shows that estrogen could play a role in the prevalence of autoimmune diseases in women. “Most women are diagnosed with lupus during childbearing years when estrogen levels are elevated,” Dr. Cadet says. “Estrogen can actually increase inflammation (which has been shown to cause and advance many common diseases) while testosterone has been thought to reduce inflammation markers.” Inflammation plays a role in many chronic diseases.
Women may be more likely to get an autoimmune disease “partly due to the role that genetics relate to the immune system or the X chromosome,” explains Dr. Cadet. “Some human and animal studies have found a gene on the X chromosome that may explain a female’s predilection to having an autoimmune disease,” But, “more studies need to be done assessing this hypothesis.”
Alexander Shikhman, MD, an integrative rheumatologist with a doctorate in infectious immunology and founder of Institute for Specialized Medicine in San Diego stresses the role of genes and immune response as contributing factors in the development of autoimmune diseases. “It is well recognized that the expression of the innate immune response in women is higher making women more prone to autoimmune disease,” explains Dr. Shikhman. “Toll-like receptors, antigen presenting cells, dendritic cells, B cells are especially higher in females.” Simply put, women have an enhanced immune reactivity (compared to men)—which makes them less susceptible to viral infections, but also predisposes them to autoimmunity due to hyper-immune responses.
What triggers autoimmune disease in women?
There are several theories as to what ultimately triggers auto-immune disease in women including infection, overly strong immune response, stress, genetics, and diet.
Studies have shown that infections may serve as an environmental trigger for autoimmunity (the misdirected immune response that makes the body attack itself). “In our practice, we always test for an underlying chronic infection that drives the autoimmune disease,” Dr. Shikhman explains. “In our experience, exposure to infectious diseases results in greater autoimmune risk in women than men; as we often see clinical manifestations of chronic infections are more acute in women.” Meaning, women are more likely to have an autoimmune reaction after an infection than men.
According to Dr. Cadet, “Women also are possibly more likely to produce more antibodies in their immune response when faced with an infection, trauma, or vaccination.” She says that “many autoimmune diseases are mediated by auto-antibodies like in RA, Sjogren’s syndrome, and lupus.” Autoimmune antibodies are groups of immune proteins that can be damaging to the body. This occurs when the immune system is confused and cannot tell the difference between “self” and “non-self” proteins. Auto-antibodies may cause inflammation and damage healthy tissues and organs, leading to an autoimmune disease.
Other possible triggers for autoimmune diseases may involve genetics, or a “Western diet,” which includes high-fat and cholesterol, high-protein, high-sugar, and excess salt and processed food intake.
Can women develop multiple autoimmune diseases?
About 25% of patients with autoimmune diseases have a tendency to develop additional autoimmune diseases. In other words, autoimmune diseases may happen in clusters.
“There is a phenomenon well known in immunology called ‘autoimmune epitope spreading,’” Dr. Shikhman explains. “It explains the development of various autoimmune processes in a given person. In response to an antigen, B cells make antibodies; the ‘best’ antibody wins and creates an attack. Over time the initial winning antibody begins to recruit other B cells producing damaging antibodies that broaden an attack on other tissues.”
Research performed at Boston Children’s Hospital and Harvard Medical school explains this process as the “runaway train” aspect of autoimmune disease. Once the autoimmune response is triggered, there is a cascade effect of autoimmune responses, which could lead to the development of additional autoimmune disorders.
Treatment for autoimmune diseases
While there is no cure for autoimmune diseases, advancements in medications are providing improved prognosis and patient functionality. Lifestyle modifications may be very helpful in reducing or mitigating auto-immune flare ups. They include:
- Stress reduction
- Healthy diet
- Exercise
- Biofeedback
- Reducing alcohol, tobacco, or other substance use
- Good sleep habits
- Healthy relationships
- Physical therapy
Medical treatment options vary for specific diseases, but may include:
- Nonsteroidal anti-inflammatory drugs (ibuprofen, naproxen): Also known as NSAIDs, these medications treat pain and reduce inflammation.
- Corticosteroids (prednisone, cortisone): These prescriptions fight inflammation and reduce immune system activity.
- Hormone replacement (insulin, levothyroxine): Autoimmune conditions such as Type 1 diabetes, and hypothyroidism require ongoing replacement of a specific hormone.
- Immunosuppressants (cyclosporine, methotrexate): These medications suppress the body’s immune system and may be used to treat lupus, rheumatoid arthritis, and psoriasis.
- Intravenous immunoglobulin: This therapy uses a mixture of antibodies to treat a number of health conditions.
- Biologics (Humira, Enbrel, Remicade, Cosentyx, Ocrevus): These medications come from living organisms and block immune pathways in cells.
The mystery of why autoimmune diseases affect women significantly more than men is multi-faceted, but as science progresses, so does the opportunity for advancement in treatments and for patients to have a better quality of life. Women who experience autoimmune disorders can achieve a high quality of life with a multifaceted treatment team and whole body approach to wellness.