Endless coughs and sneezes, runny noses, and unexplained itchy bumps—kids seem to be a magnet for germs. In our parent’s guide to childhood illnesses, we talk about the symptoms and treatments for the most common conditions. Read the full series here.
What is ringworm? | Symptoms | Ringworm vs. other rashes | Diagnosis | Treatments | Prevention
True or false: Ringworm is caused by a creepy crawly that burrows under the skin? Most people are surprised to find out that this condition has nothing to do with worms. Rather, it’s a contagious skin infection that easily spreads after direct contact with an infected area. It’s common—at least 20% of people have at least one infection in their lifetimes—but it’s also treatable, usually without serious complications.
What is ringworm?
Ringworm, also known as tinea or dermatophytosis, is a fungal infection that affects the skin and nails. There are 40 different species that cause ringworm, falling into three genuses: Trichophyton, Microsporum, and Epidermophyton. The condition gets its name from its hallmark symptom: a round, itchy rash.
“It can present on almost any part of the body except for the mucosal skin,” says Anna H. Chacon, MD, a board-certified dermatologist based in South Florida, who serves on the advisory board for Smart Style Today. “I have seen it on the face, genitalia, trunk, extremities, and scalp. It can have varying degrees of severity.” The infection is referred to differently depending on where it presents.
According to the U.S. Centers for Disease Control and Prevention (CDC), it’s called:
- Tinea pedis on the feet (commonly referred to as athlete’s foot)
- Tinea cruris on the groin area, inner thighs, or buttocks (commonly referred to as jock itch)
- Tinea capitis on the scalp
- Tinea barbae on the beard (commonly referred to as barber’s itch)
- Tinea manuum on the hands
- Tinea unguium on toenails and fingernails
- Tinea corporis on other parts of the body, such as arms or legs
Ringworm of the scalp and body are the most common types of ringworm in young children. The other forms are rare before puberty: They generally affect teens and adults.
There are 40 different species that cause ringworm, falling into three genuses: Trichophyton, Microsporum, and Epidermophyton.
How do you catch ringworm?
“Ringworm is spread through direct contact—often from person to person, contaminated surface to person, or pet to person,” says Ashanti Woods, MD, a pediatrician at Mercy Medical Center in Baltimore. “Often one touches a contaminated surface and has the fungus on their hand. They then scratch themselves and embed the fungus that was on their hand into their skin.”
Ringworm infections often occur in schools, childcare centers, community gyms, and pools. It can be carried on any surface, but some of the highest risks include:
- Surfaces that are wet or damp
- Towels, combs, brushes, hats, and other personal items
- Gym mats
- Shared spaces that tend to be warm and moist, such as bathrooms and locker rooms
Other risk factors for contracting ringworm include:
- Living in a warm humid climate
- Malnourishment
- Poor hygiene
- Playing contact sports (particularly wrestling as it involves skin to skin contact)
- A weakened immune system (through illness or medication)
While ringworm can take several weeks to fully cure, it is no longer spread to others after 48 hours of treatment. Children do not need to miss school or daycare for ringworm, but if possible, it is a good idea to cover the affected area with clothing or a loose bandage during the infectious period to prevent potential spread to other children or caregivers.
Ringworm symptoms in children
Ringworm gets its name from the rash’s “worm-like” appearance. “Typically, ringworm starts off as a red pimple that grows out into a ring with a raised border and smooth clear central area,” Dr. Woods says. “Ringworm of the scalp typically leads to bald patches with crusting or flaking/scaling of the skin. Occasionally, the lymph nodes closest to the area of inflammation will swell up and may become painful to touch.”
Symptoms of ringworm of the body include:
- Ring-like rash with a raised edge
- The center of the ring often becomes less red as the lesion gets bigger
- Itchiness in the rash area
On light-colored skin, patches usually appear red or pink. On dark-colored skin, patches tend to be brown or gray. Patches can appear in one or multiple areas and grow slowly in size.
Symptoms of ringworm of the scalp include:
- Patchy, flaky, or scaly patches or sores
- Hair loss that causes bald patches or blisters
- Itchiness or tenderness of the scalp
If the patches become infected, they can become a kerion, a pus-filled mass that leads to swollen and tender lymph nodes in the head and neck.
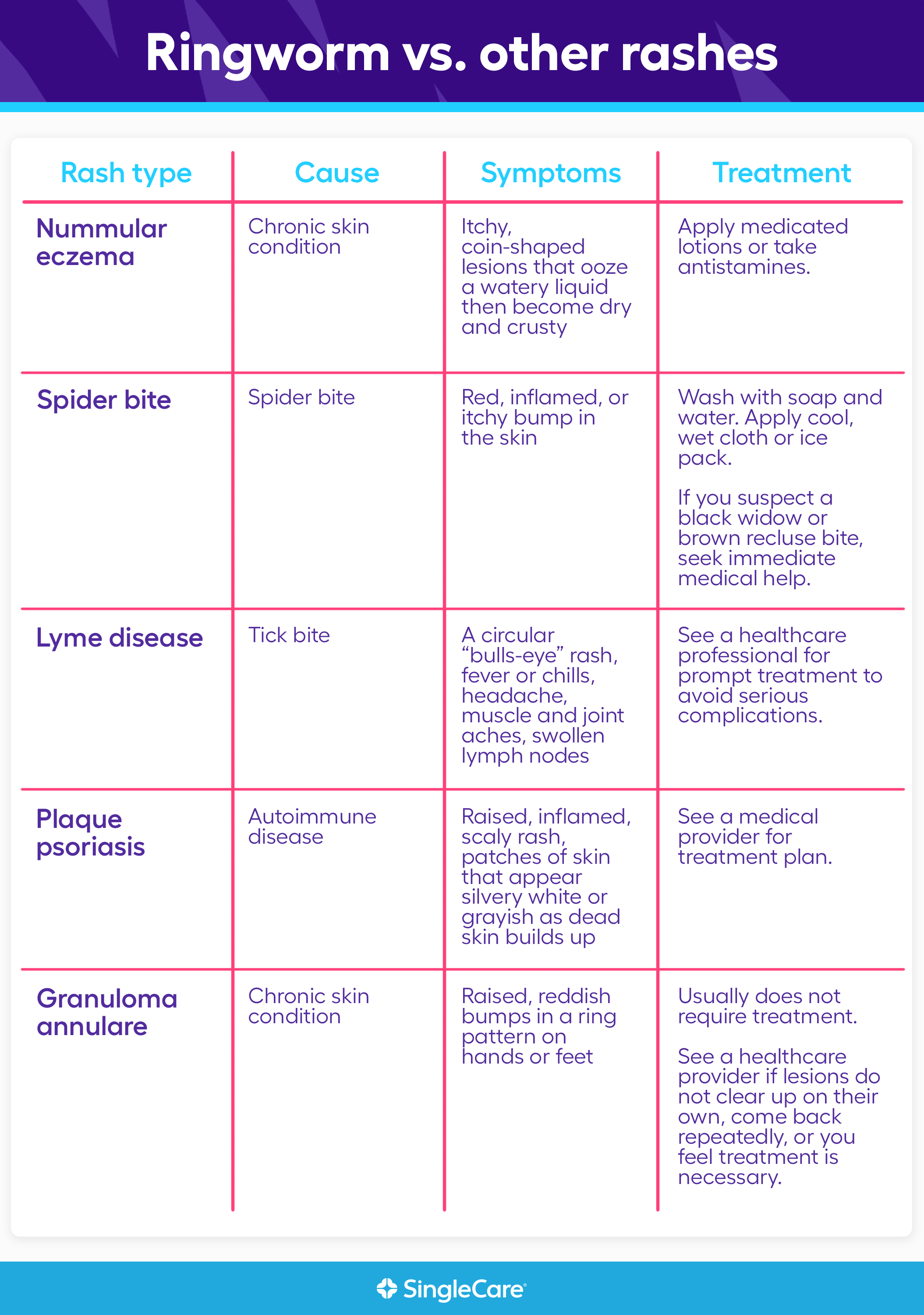
Ringworm vs. other rashes
These are some conditions that can be mistaken for ringworm, in order of most common to least common. When in doubt, make an appointment with your child’s primary care provider to confirm the diagnosis.What should I do if suspect my child has ringworm?
What should I do if suspect my child has ringworm?
“[Diagnosis of ringworm] can be made by examination alone,” says Dr. Woods. “Occasionally, a physician or nurse practitioner may take a skin scraping or skin culture to confirm it’s ringworm.” The provider may also look at the rash under a black fluorescent light.
Because other conditions can mimic ringworm, it’s a good idea to see a healthcare professional to confirm a diagnosis. Ringworm can be diagnosed by a general practitioner (family doctor), nurse practitioner, dermatologist, or pediatrician.
Contact a healthcare provider within 24 hours if pus is present, the rash is warm to the touch, painful, or has streaking beyond the initial lesions, or if your child had a recent tick bite and a rash that looks like ringworm appears.
Contact a healthcare provider during office hours if:
- Your child has a fever 101 or greater.
- Your child is less than 12 months old.
- You are unsure if the rash is ringworm.
- The scalp is involved.
- The rash gets bigger or spreads after one week of treatment.
- More than three lesions are present.
- The rash lasts longer than four weeks.
- Your child has a weakened immune system.
- Your child participates in contact sports.
Treatments for ringworm in kids
“Sometimes the body can clear ringworm on its own,” says Susan Bard, MD, a dermatologist at Vive Dermatology in Brooklyn, New York. “But oftentimes [ringworm] will require medical intervention.”
Ringworm of the body
In many cases, ringworm of the body can be treated at home with over-the-counter (OTC) medications, without involvement of medical professionals—but it is not possible to get rid of ringworm fast.
“The treatment for ringworm of the body is an OTC topical antifungal such as clotrimazole cream (Lotrimin),” Dr. Woods says. “It is applied to the affected area twice a day for four weeks.”
Common antifungal creams for treatment of ringworm include:
- Desenex, DermaFungal, and Micaderm (miconazole)
- Lamisil (terbinafine)
- Lotrimin, Mycelex (clotrimazole)
- Xolegel (ketoconazole)
Ringworm of the scalp
Ringworm of the scalp requires a prescription from a healthcare professional, and treatment usually lasts one to three months. “Ringworm of the scalp is treated with oral antifungal medicines and topical antifungal shampoo,” says Dr. Woods.
Prescription antifungal medications used to treat ringworm of the scalp include:
- Diflucan (fluconazole)
- Grifulvin V, Gris-PEG (griseofulvin)
- Onmel, Sporanox (itraconazole)
- Terbinafine
While ringworm can frequently be treated with OTC medications, home remedies are not effective.
How to prevent ringworm in kids
It is common for ringworm to recur, and it can spread to other members of the household. Some ways to ensure a ringworm infection clears up completely, and to help prevent its spread to other family members include:
- Use all medication as directed, and for as long as is recommended—even if the ringworm appears to be gone.
- Treat all ringworm at the same time (areas of the body, and people in the house who are infected). In the case of ringworm of the scalp, it is helpful to have the whole household use the antifungal shampoo whether or not they are showing symptoms.
- Practice proper handwashing—especially those who have touched the area affected by ringworm, such as the child and the person administering treatment.
- Keep your child’s body clean and dry, especially the area affected by ringworm. Develop good hygiene habits such as regular bathing, and gently towel off after every shower, bath, or swim. (Use a different towel for the affected area than for the rest of the body.) If your child has recurrent infections, consider drying specific areas (groin, between toes) with a hair dryer on the cool setting. Keep up this practice even once the ringworm is gone to help prevent a recurrence.
- Have your child wear breathable clothing (clothes that don’t make the child sweat), and change their clothes (including socks and underwear) every day.
- Encourage your child to shower when sweaty, and avoid sharing towels or other personal items such as hats, combs, and headbands. Use shower shoes in communal bathrooms or public places.
- Disinfect or throw out items that may be contaminated from contact with an infected person. Ringworm can live on surfaces for a long time.
- Watch your pet for signs of ringworm, and take it to the vet if any are observed. If ringworm keeps recurring, it would be a good idea to have your pets examined to see if they are the source of the infections.
Ringworm is unpleasant and stubborn. It’s easy to catch, hard to get rid of, and is generally a nuisance. Thankfully, with OTC and prescription medication, it usually goes away fully, and without lasting effects.











