Pulmonary embolism symptoms: What are the early signs of pulmonary embolism?
Overview: What does pulmonary embolism feel like?
A pulmonary embolism is a blood clot stuck in the lung’s arteries. The clot blocks blood from flowing to the lungs to pick up oxygen to carry to the rest of the body. Usually, the blood clot forms in the legs (called deep vein thrombosis or DVT). It then breaks and travels to the arteries in the lungs. A pulmonary embolism (PE) is a potentially life-threatening medical emergency. Prompt treatment is critical. If untreated or caught too late, 30% of people with PE will die, but more than 90% will survive if caught and treated in time. Unfortunately, the symptoms of pulmonary embolism are also common signs of other medical conditions.
How does it feel? Usually, it feels hard to breathe, but the severity is highly variable. It may not be too hard to breathe, or it may seem like a desperate struggle. Typically, people breathe faster, and their chest may hurt. They cough, sometimes coughing up blood. Some people will have no symptoms or mild symptoms, even with a severe pulmonary embolism. Some people are only diagnosed by accident.
Key takeaways:
Pulmonary embolism is a rare health condition that can affect anyone regardless of age, sex, race, or ethnicity.
Early signs of pulmonary embolism include problems breathing, fast breathing, and chest pain.
Serious symptoms of a pulmonary embolism, such as severe chest pain, severe breathing problems, fainting, low blood pressure, and coughing up blood, require immediate medical attention.
A pulmonary embolism is caused by a blood clot, usually one that forms in the legs. You may be at risk for developing pulmonary embolism symptoms if you have a history of blood clots or a family history of blood clots. Recent orthopedic surgery, hip or knee replacement, lower limb fracture, injury, or deep vein thrombosis could also raise your risk. Medical conditions such as congestive heart failure, respiratory failure, and obesity increase the prevalence of pulmonary embolism too. Hormones contribute to the elevated risk associated with birth control pills and during pregnancy. Modifiable risk factors include smoking and being sedentary.
Pulmonary embolism requires a medical diagnosis.
Symptoms of pulmonary embolism generally do require treatment. They typically resolve with treatment within a few months, but not always.
Treatment of pulmonary embolism may include supportive treatment, anticoagulants, drugs that break up blood clots, or surgery to break up the blood clot.
Untreated pulmonary embolism could result in complications like high blood pressure in the pulmonary arteries, recurrent blood clots, heart failure, cardiogenic shock (clot blocks the ability of the heart to provide adequate circulation), cardiac arrest, and death.
Save on prescriptions for pulmonary embolism with a SingleCare prescription discount card.
What are the early signs of pulmonary embolism?
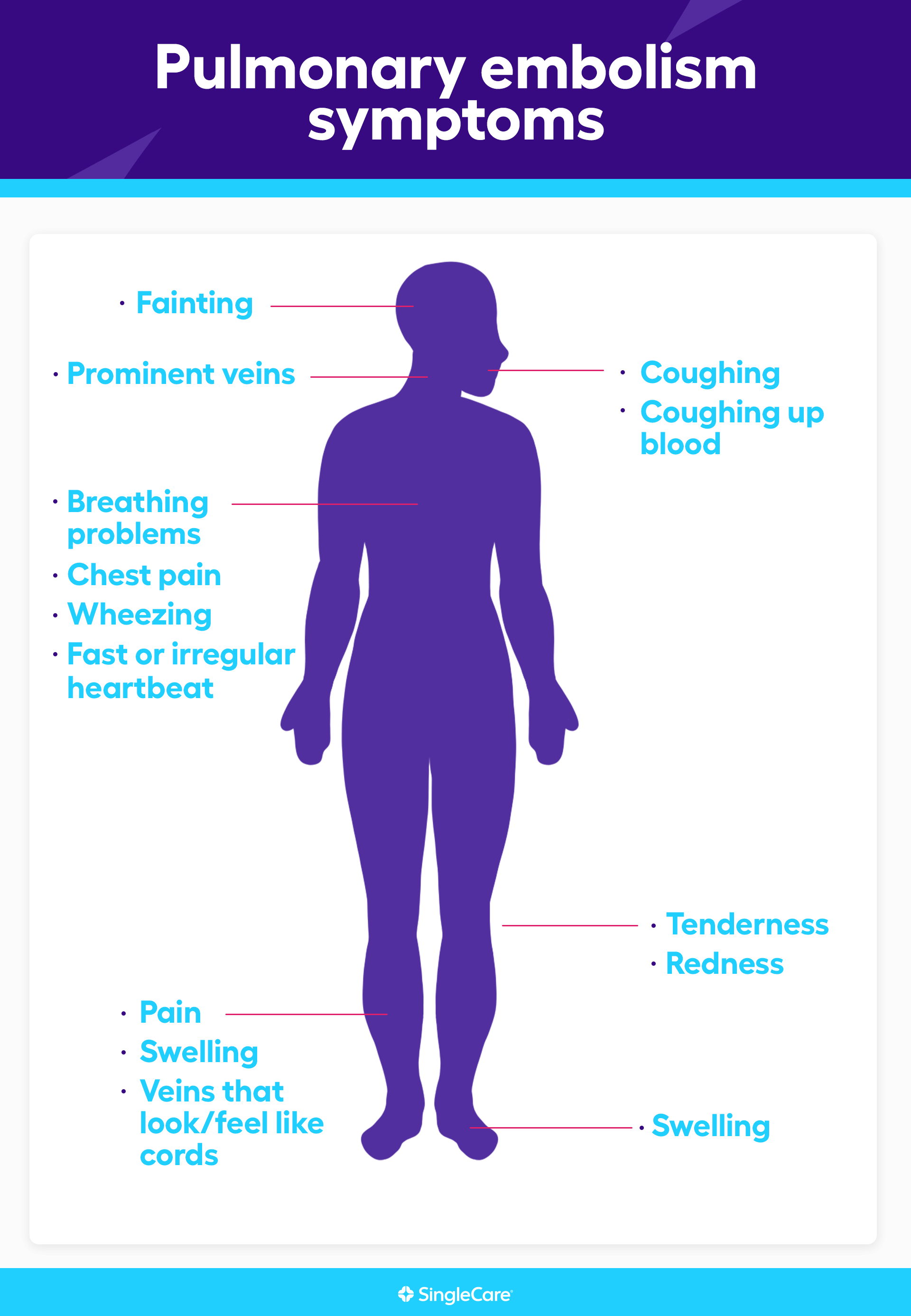
The most common signs of pulmonary embolism are:
Breathing problems
Fast breathing
Chest pain that worsens with breathing
Coughing
Some people will have only minor symptoms or no symptoms at all.
Other pulmonary embolism symptoms
The symptoms of pulmonary embolism are not very specific; that is, they can also be signs of other medical conditions.
Pulmonary embolism symptoms include:
Difficulty breathing (73% of patients with PE)
Pain that worsens when breathing (66%)
Coughing (37%)
Calf or thigh swelling (28%)
Calf or thigh pain (26%)
Coughing up blood (13%)
Wheezing (9%)
Fast breathing
Fast heartbeat
Feeling faint
Fainting
Heartbeat irregularities
Foot swelling
Tenderness of lower extremity
Prominent neck veins
Skin redness of lower extremity
Calf or leg veins that look and feel like cords
Severe pulmonary embolism can cause blood pressure to fall, a clear sign that something is seriously wrong. Symptoms of low blood pressure include:
Dizziness
Lightheadedness
Fainting
Fatigue
Blurred vision
Heart palpitations
Problems with thinking or concentration
Confusion
Nausea
Cold and pale skin
Fast breathing
RELATED: What happens when your blood pressure is too low
Pulmonary embolism vs. fat embolism symptoms
A fat embolism is a globule (embolus) of fat that gets into the circulatory system (usually more than one). They’re not big enough to cause blockage in an artery or vein, but they can disrupt blood flow through tiny blood vessels. Bone fractures are a common source of these fat globules, but surgery and liposuction can also cause the problem. Unlike PE, fat globules can cause problems in any body organ. If enough fat gets into the bloodstream, many organs are affected, typically the skin, the brain, the eyes, the heart, and the lungs. This condition is called fat embolism syndrome (FES), so problems throughout the body are one way to distinguish it from a pulmonary embolism. However, a fat embolism is even more challenging to diagnose than a pulmonary embolism.
| Pulmonary embolism | Fat embolism | |
| Shared symptoms |
|
|
| Unique symptoms |
|
|
Types of pulmonary embolism: How can I tell which one I have?
Healthcare professionals classify pulmonary embolism in two ways, but the most important distinction involves blood pressure. Low blood pressure is a bad sign and means the condition is potentially life-threatening. The technical terms are “hemodynamically stable” for PE patients with normal blood pressure and “hemodynamically unstable” for those whose blood pressure has dropped significantly. Low blood pressure has identifiable symptoms such as dizziness, lightheadedness, confusion, and fainting. Always get immediate medical care when blood pressure drops too low.
Healthcare professionals also classify pulmonary embolism based on where the blood clot has gotten stuck in the lung. This classification requires a CT scan or other medical imaging, so it’s not something people can identify by themselves.
When to see a doctor for pulmonary embolism symptoms
See a doctor if there’s any suspicion that you or a loved one have symptoms indicating a pulmonary embolism. Some symptoms are signs that emergency medical treatment is needed no matter what the cause, including:
Low blood pressure
Severe chest pain
Persistent or severe breathing problems
Coughing up blood
A doctor will take a medical history, perform a physical exam, and measure oxygen levels in the blood. It’s important to share all your health information with the doctor, especially:
Any history of blood clots, especially deep vein thrombosis or pulmonary embolism
Any recent surgery
Any recent bone break
Any recent period of lengthy immobilization
Active cancer
Birth control or estrogen use
Leg swelling
The doctor will score the medical history, symptoms, and results of the physical exam to determine the likelihood of a pulmonary embolism.
If the probability is high, the doctor may order blood tests, a d-dimer test (to indicate blood clots), an electrocardiogram (EKG) to measure heart function, and imaging tests such as a chest X-ray, CT scan, pulmonary angiogram, MRI, or ventilation-perfusion scan (V/Q scan), which allows the doctor to see blood flow in the lungs without using high levels of radiation. An echocardiogram of the heart and an ultrasound image of the lower legs may be needed.
Complications of pulmonary embolism
Both treated and untreated, a pulmonary embolism can cause significant complications including:
High blood pressure in the lung’s arteries (pulmonary hypertension)
Recurrent blood clots
Heart failure
Cardiogenic shock (the heart loses the ability to pump enough blood to the body)
Cardiac arrest
Death
How to treat pulmonary embolism
To avoid serious complications and death, a pulmonary embolism requires early and intense treatment. The primary focus is getting blood pressure back to normal, preventing the blood clot from getting bigger, stopping other blood clots from forming, and breaking up the blood clot. To do this, doctors may use:
Anticoagulants: drugs such as heparins to prevent the clot from growing or new clots from forming
Fluids: intravenous fluids can help bring blood pressure back to normal
Clot dissolvers (thrombolytic therapy): intravenous drugs that break apart blood clots
Catheter thrombolysis: the doctor may insert a catheter into the involved artery to infuse a clot-dissolving medication into the blood clot
Surgical removal of the blood clot: in very severe cases, the surgeon will cut open the chest and remove the blood clot
Vena cava filter: sometimes the doctor will insert a catheter and place a filter in the vein entering the heart (the inferior vena cava) to prevent more blood clots from entering the lungs
Preventing recurrent pulmonary embolisms
Once the crisis is over, the new reality is that pulmonary embolism, deep vein thromboembolism, and other blood clot problems are more likely to recur than in other people. After the event, anticoagulant treatment will continue for at least three months and possibly longer to prevent a recurrence. To prevent problems in the future, anyone who has gotten through a pulmonary embolism should:
Take all prescribed medications as directed
Follow the medical advice and diet prescribed or suggested by the doctor
Keep all follow-up appointments with healthcare professionals
Make sure all healthcare providers and doctors know that you have had a pulmonary embolism
Wear compression stockings if instructed
Know the symptoms of deep vein thrombosis and pulmonary embolism and get medical attention if they occur
RELATED: Is it safe to drink alcohol when taking blood thinners?
Most importantly, see a doctor as soon as symptoms begin
Prompt treatment is required to prevent the worst outcomes of pulmonary embolism. Be aware of high-risk factors such as birth control pill use, long-term bed rest, or a broken bone.
Educate yourself about deep vein thrombosis and pulmonary embolism and their symptoms. If you experience signs of PE or DVT, get medical attention immediately. Only a doctor can definitively diagnose a pulmonary embolism and treat it promptly.
FAQs about pulmonary embolism symptoms
What are the early warning signs of a pulmonary embolism?
The most common signs of a pulmonary embolism are breathing problems, fast breathing, chest pain, and coughing. However, some people may have no warning signs or mild symptoms.
How long can you have a pulmonary embolism without knowing?
Pulmonary embolism symptoms can be mild. Sometimes there are no symptoms, even if the pulmonary embolism is severe. No matter what the symptoms, a pulmonary embolism is a life-threatening illness. Left untreated for too long, a pulmonary embolism has a mortality rate of 30%.
What does a pulmonary embolism feel like?
A pulmonary embolism can sometimes feel like nothing, but most people will experience some signs and symptoms. The most common is difficulty breathing. It can range from shortness of breath with exertion to a real struggle to breathe, even when sitting or lying down. Other common symptoms include fast breathing, chest pain, and coughing.
What’s next? Additional resources for people with pulmonary embolism symptoms
Test and diagnostics
Acute pulmonary embolism, StatPearls
Pulmonary embolism symptoms and diagnosis, American Lung Association
Treatments
Acute pulmonary embolism, StatPearls
Deep venous thrombosis and pulmonary embolism: current therapies, American Family Physician
Treating and managing pulmonary embolism, American Lung Association
Scientific studies and clinical trials
Clinical characteristics of patients with acute pulmonary embolism, The American Journal of Medicine
Surgical embolectomy for acute pulmonary embolism: state of the art, Journal of Thoracic Disease
More information on related health conditions
Deep vein thrombosis treatments and medications, SingleCare
Fat embolism, StatPearls
What happens when your blood pressure is too low, SingleCare
Chad Shaffer, MD, earned his medical doctorate from Penn State University and completed a combined Internal Medicine and Pediatrics residency at the University of Pittsburgh Medical Center and Children’s Hospital of Pittsburgh. He is board certified by the American Board of Internal Medicine and the American Board of Pediatrics. He has provided full-service primary care to all ages for over 15 years, building a practice from start up to over 3,000 patients. His passion is educating patients on their health and treatment, so they can make well-informed decisions.
...Related Drugs
Related Drug Information
Popular Prescriptions
Subscribe to our savings newsletter
Health education, drug info, wellness & more
SingleCare is a prescription discount service that offers free coupons on thousands of prescription drugs. It can be used whether you have insurance, Medicare, Medicaid, or none of the above, but it cannot be combined with insurance.
SingleCare provides transparent drug pricing, so you can compare discounts at pharmacies near you. Browse singlecare.com to find drug discounts, helpful information about your prescription, and resources to help you make informed health decisions.
Prescription savings vary by prescription and by pharmacy, and may reach up to 80% off cash price. This is a medical discount plan. This is NOT insurance. This program offers you the opportunity to locate providers of various types of medical services who will offer their services to you at discounted rates. The range of discounts for medical or ancillary services provided under the plan will vary depending on the type of provider and service received. You are fully responsible for paying for all health care services but will be entitled to receive a discount from those health care providers in accordance with the specific pre-negotiated discounted fee schedule. This program does not guarantee the quality of the services or procedures offered by the providers. Except for prescription drugs which you will pay directly to the pharmacy at the time of purchase, all other services received through a program provider will be charged to the credit card on file in your member account. The charge will include an administrative fee for use of the program. Towers Administrators LLC is the licensed discount medical plan organization with its administrative office located at 4510 Cox Road, Suite 111, Glen Allen, VA 23060. SingleCare Services, LLC is the marketer of the discount medical plan organization including its website, singlecare.com, with its corporate office located at 99 High Street, Suite 2800, Boston, MA 02110. For additional information, including an up-to-date list of providers, or assistance with any issue related to program membership, please contact member support any time at www.singlecare.com, or by calling toll-free 844-234-3057, 24 hours, 7 days a week (except major holidays). Pharmacy names, logos, brands, and other trademarks are the property of their respective owners.
Blog articles are not medical advice. They are intended for general informational purposes and are not meant to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. If you think you may have a medical emergency, immediately call your physician or dial 911.
© 2026 SingleCare Administrators. All rights reserved
© 2026 SingleCare Administrators. All rights reserved







