Polycystic ovary syndrome, commonly referred to as PCOS, is a complex hormonal disorder that affects approximately 6-12% of women in the United States during their reproductive years. It’s also one of the most common reasons behind infertility, according to the Centers for Disease Control and Prevention (CDC), but it’s cause is largely unknown. That makes it difficult to pinpoint the best PCOS treatment.
What are the symptoms of PCOS?
Due to an imbalance of hormone levels in the ovaries, common indicators of PCOS include missed or irregular periods, extremely heavy menstrual periods, and/or the inability to release eggs (or ovulate). An interrupted menstrual cycle can lead to other symptoms and side effects, such as cysts in the ovaries. Also, if a woman with PCOS has an abundance of the male hormone androgen, her body will likely respond by growing excess body and facial hair, along with possibly developing severe acne and male-pattern baldness. Weight gain is also a sign of PCOS.
“PCOS isn’t life-threatening, but it can make life quite annoying,” says Shweta Patel, MD, an OB/GYN at Orlando Health Physician Associates in Orlando, Florida. “It can lead to some very unappealing and outwardly obvious symptoms and make your ovulatory window a moving target, thus making it more difficult—but not impossible—to conceive in a timely fashion.”
What causes PCOS?
As many as 5 million women suffer from polycystic ovarian syndrome, but the cause is largely unknown. A few common risk factors include:
- genetics
- obesity
- high insulin levels (a protein that helps regulate blood sugar levels)
- high androgen levels
A 2018 study published online in the International Journal of Environmental Research and Public Health concluded that neither ethnicity nor geographic location play a role in PCOS.
Are there other conditions associated with PCOS?
However, research indicates that numerous health conditions are associated with this syndrome—even though it has yet to be determined if PCOS causes these issues or vice versa. The Office on Women’s Health (which is run by the U.S. Department of Health & Human Services) lists the six long-term health problems associated with PCOS:
- Diabetes: More than 50% of women diagnosed with PCOS develop diabetes or pre-diabetes by the age of 40, states the CDC.
- Hypertension: Women with PCOS are at an increased health risk of having high blood pressure, which can lead to cardiovascular disease.
- Hypercholesterolemia: Women with PCOS are more likely to have higher levels of LDL (“the bad”) cholesterol compared to females without PCOS.
- Sleep apnea: Women with PCOS are at higher risk of developing this respiratory disorder, in which momentary breathing pauses interrupt sleeping. This condition can lead to heart disease and diabetes.
- Depression and anxiety: A 2016 systematic review and meta-analysis published in the journal Neuropsychiatric Disease and Treatment found that women with PCOS are about three times more likely to suffer from anxiety compared to women without PCOS. The results were similar for those diagnosed with PCOS and depressive symptoms.
- Endometrial cancer: A 2018 population-based cohort study published in the journal Medicine concluded that women with PCOS had a “statistically significant higher risk” of developing cancer of the uterus.
Is PCOS curable?
PCOS tends to be a disorder that can be managed rather than cured since it often recurs, especially if the patient gains (or regains) body weight and/or is diagnosed with diabetes, explains Jessica Shepherd, MD, an OB/GYN with Minimally Invasive Gynecology at Baylor University Medical Center in Dallas, Texas. Since symptoms vary, Dr. Patel adds that she tends to “tailor the treatment to the goals of the patient.”
How is PCOS treated?
You can treat PCOS with a combination of the following lifestyle changes and medications. Here are five PCOS treatment options you may consider.
1. Diet
Dr. Shepherd says that changing your eating style (perhaps to a low-fat plan) will help shed unwanted pounds. In some cases, weight loss can improve insulin sensitivity, menstrual function, and boost fertility. “Also, diet modification can help with insulin resistance and decrease the chances of it becoming a metabolic issue, which can lead to diabetes, hypercholesterolemia, or hypertension,” she continues.
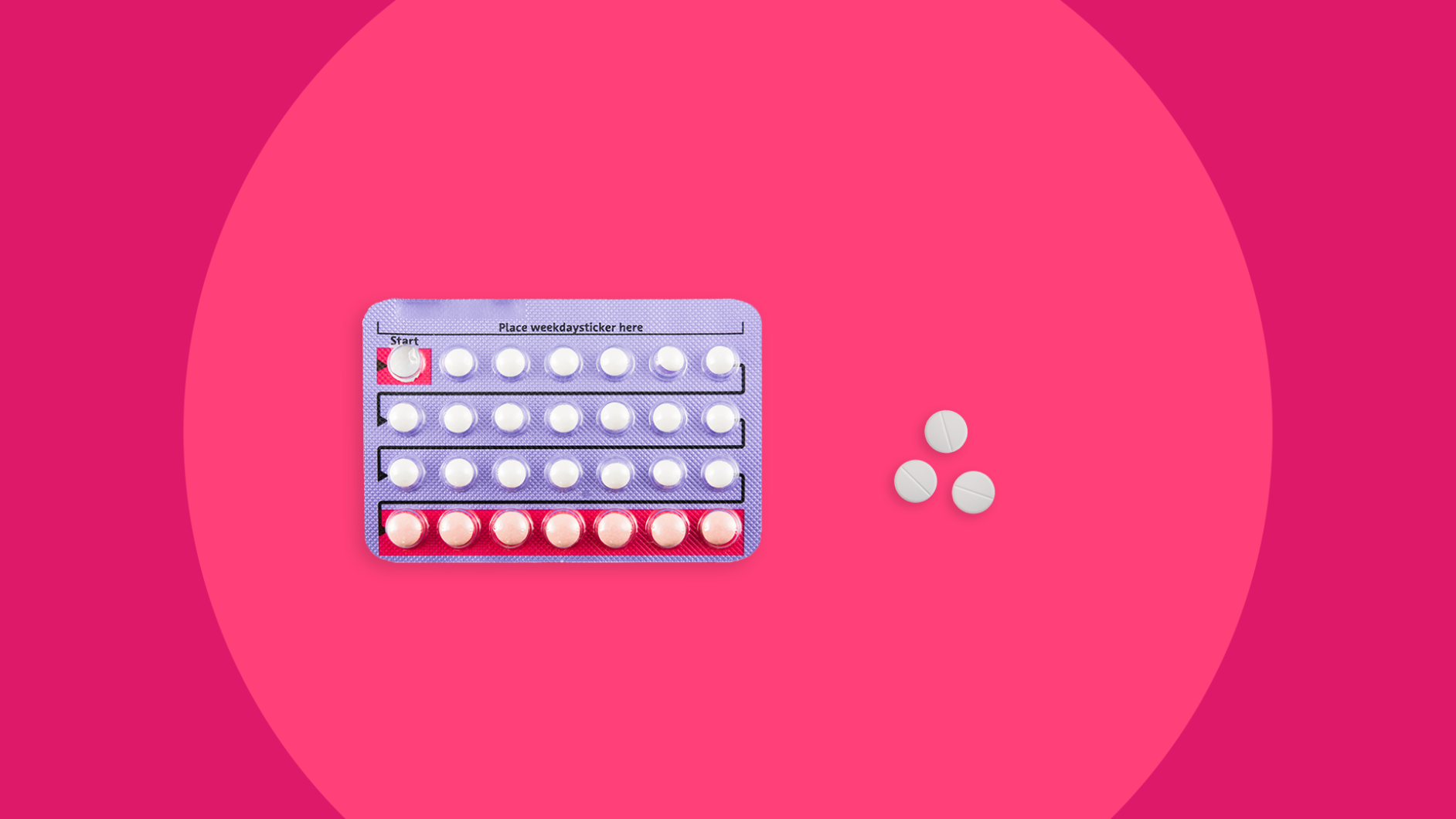
2. Birth control
For women who are not looking to conceive, oral contraceptives can “help to regulate periods and also give cyclic estrogen, which is often disrupted,” Dr. Shepherd says. A gynecologist might prescribe combination birth control pills or other forms of contraception that contain both estrogen and progestin (such as a vaginal hormonal ring) to minimize abnormal bleeding, reduce excess hair growth, lessen acne, and decrease the risk of endometrial cancer.
3. Metformin
“Metformin [an anti-diabetic medication] has been shown to induce resumption of normal, ovulatory menstrual cycles in 40-90% of patients studied,” Dr. Shepherd states. She adds that this prescription medication may also improve fertilization and pregnancy rates in women with PCOS, though it’s use for this indication is considered off-label and should be discussed with your doctor. An oral med which belongs to a class of drugs called biguanides, metformin is designed to increase the body’s response to insulin in order to balance glucose levels in people diagnosed with type 2 diabetes. A 2015 study published in the journal Diabetes Care discovered that this medication can also reduce LDL cholesterol levels. Glucophage is a popular brand name of metformin.
RELATED: Metformin for off-label treatment of PCOS
4. Anti-androgen medications
A type of therapy used to block androgens (aka “male” sex hormones including testosterone), these drugs can help decrease any male characteristics related to PCOS, such as acne, unwanted hair, and a receding hairline. “Treating excessive androgens can also be accomplished by using spironolactone [a diuretic typically prescribed to treat high blood pressure which has anti-androgenic effects], either on its own or in conjunction with a birth control pill,” Dr. Patel states. And Dr. Shepherd adds that “decreasing testosterone action can reduce hirsutism [male-pattern hair growth on women] scores by 40%.” The Office on Women’s Health warns that this class of meds can cause complications during pregnancy. You might also ask your endocrinologist about Vaniqa, which is a topical hair removal cream.
5. Estrogen modulator
In order to treat infertility, Dr. Patel says that physicians often prescribe an estrogen modulator, such as clomiphene citrate—an oral medication commonly known as Clomid, which belongs to a category of drugs called ovulatory stimulants. It works similar to estrogen by encouraging the ovaries to develop and release eggs. A 2015 article published in the journal Clinics reported that women with PCOS who used clomiphene citrate as a first-line pharmacological treatment for infertility had a 70% pregnancy rate.