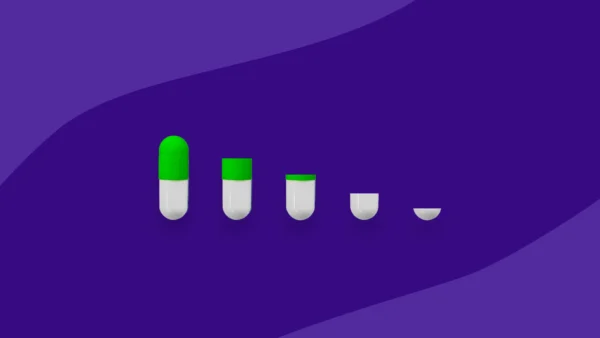
Swallow a pill, wait a little while, feel better—simple, right? Not exactly.
What is the ADME process?
A drug’s journey through your body—a discipline within pharmacology called pharmacokinetics—is anything but simple. From the time the drug goes into your body to the time it leaves, a lot happens. Scientists have dubbed the process ADME, short for absorption, distribution, metabolism and, finally, excretion. But how, exactly, does a drug go from point A (absorption) to point E (excretion)? We asked the experts.
Absorption
Absorption depends a lot on the drug’s delivery system. Injectables bypass the absorption phase because they’re delivered directly to the bloodstream. But most medications we take at home are in pill or capsule form, and those need to be absorbed in the stomach or gastrointestinal tract (gut). In scientific speak, the drug needs to become “soluble” before it can gain access to the circulatory system.
Sounds straightforward, but, like a lot of things in medicine, it isn’t. The acidity of the stomach and gut, as well as the makeup of the drug itself, can impact absorption. Ditto for the fillers and coatings used in the drug’s making.
“The stomach has an acidic environment,” explains Colin Campbell, Ph.D., an associate professor of pharmacology at the University of Minnesota Medical School in Minneapolis. “What we call weak acid drugs, like aspirin, are well-absorbed there. But a weak base drug, like morphine, has slower absorption because, unless it’s given by injection, it has to get from the high-acid environment of the stomach to the more neutral environment of the gut for absorption.”
Distribution
After a drug gains access to the bloodstream, the blood “distributes” it to the body’s tissues.
How that happens depends a lot on the drug’s properties.
For example, fat-soluble drugs (like prednisone, a steroid used to treat inflammation) seek out fat cells where they easily dissolve and pass through cell membranes. Water-soluble drugs, such as atenolol, used to treat high blood pressure, stick around in the blood and the fluids surrounding cells.
Another factor affecting distribution is whether the drug is made up of large or small molecules. Most drugs used therapeutically are small molecule drugs—and for good reason. Small molecule drugs, such as Nexium (used to treat gastroesophageal reflux disease), pass easily through cell membranes so they can continue their journey. Large molecule drugs, such as insulin, have a harder time permeating membranes and are best given by injection.
Metabolism
Metabolism, also called biotransformation, generally happens in the liver.
During distribution, the drug is transported to the liver through a natural process or with the help of what’s called “transporters” that exist on the cells of organs. Special enzymes located in the liver chemically alter the drug and transform it into a form that can be easily excreted.
But there’s a catch. Issues affecting the liver can impact how fast a drug is broken down. Cirrhosis (or scarring of the liver), for example, can make it harder for a drug to be metabolized, letting it remain in the body longer. A few drugs are metabolized in the kidneys as well.
And some drugs can inactivate the metabolizing enzymes or transporters, says Joseph Grillo, Pharm.D., associate director for labeling and health communication in the Office of Clinical Pharmacology at the FDA. “This can result in the drug remaining in the body longer and in greater amounts than necessary, increasing the chances of toxicity,” he says.
Excretion
Excretion is the process by which the body rids itself of a drug, and that’s mostly handled by the kidneys and the urine they produce. If a drug is not easily filtered by the kidneys, it can sometimes be altered by the liver so remnants can pass via urine. Drugs that aren’t able to be filtered by the kidneys pass through the biliary ducts in the liver and leave the body by way of the feces.
Beyond ADME: What you need to know
A lot of factors affect how your body processes a drug. For starters, there’s:
- Age. Older organs don’t operate as efficiently as younger ones, which means the way your liver, stomach, or kidneys processed a drug at 25 is different than at 65. The amount of drugs older people take can also affect the process.
- Gender. Because we differ in body weight, fat, volume of body water, blood flow to organs and hormone levels, ADME can be different in men and women.
- Stomach contents. No big shocker here―that cheeseburger and fries you ate after taking your medication can slow down a drug’s journey. “Most foods are better absorbed through the gut,” says Campbell. “But a full stomach will slow absorption and take the drug longer to move to the gastrointestinal system.” On the other hand, some medications should be taken with food for better absorption.
Bottom line? Follow directions. “Read the prescription bottle label and any inserted material carefully, and ask questions if you need clarification,” Dr. Grillo says.