Normal blood oxygen levels | Blood oxygen level chart | How to check blood oxygen | Risk factors | COVID-19 | Symptoms of low blood oxygen | When to see a doctor | How to increase blood oxygen levels
It’s always important to pay close attention to your body and overall health. And as viruses like the common cold, the flu, and COVID-19 continue to circulate, your risk of secondary respiratory infections and breathing problems increases, too. When it comes to assessing your current health status, medical experts typically check your body temperature, pulse, blood pressure, and breathing rate. But your blood oxygen levels are important too—they measure the amount of oxygen you have circulating in your blood.
Here’s a look at blood oxygen levels, what affects them, what’s considered normal, and how to increase yours.
Normal blood oxygen levels
Blood oxygen levels are often classified as low, normal, or high, and typically range from 75-100 millimeters of mercury (mmHG). Normal readings typically fall between 95-100 mmHG for both adults and children. For example, an oxygen level of 94 would be considered normal and healthy. Anything lower than 90 is considered low.
Keeping your blood oxygen level in a normal range is critical to your health. When this level dips below the normal range, medical attention is necessary. “Patients can develop an individualized baseline blood oxygen saturation that, when significantly altered, can alert them to seek medical attention,” says Shahyar Yadegar, MD, critical care medicine specialist, pulmonologist, and medical director of the ICU at Providence Cedars-Sinai Tarzana Medical Center. For individuals with a chronic lung disease, normal blood oxygen levels may be lower.
Low blood oxygen levels put you at risk of developing hypoxemia, which the Mayo Clinic defines an arterial blood oxygen level below 75mmH. If that value dips under 60 mmHG, supplemental oxygen is necessary. Having a below-normal blood oxygen level also puts you at risk of developing hypoxia, or low oxygen in your tissues. These are two different conditions, but they can present with similar symptoms.
Your provider may want to measure your blood oxygen levels in the following situations:
- You’re having trouble breathing; for example you can’t speak full sentences or complete small tasks without difficulty breathing.
- You’re undergoing treatment for a lung disease like asthma, chronic obstructive pulmonary disease (COPD), or cystic fibrosis. The test can help to see if treatment is working.
- You have a recent head or neck injury that’s impacting your breathing.
- You’ve had a drug overdose.
- You’re undergoing oxygen therapy during a hospital stay.
- You have carbon monoxide poisoning.
- You’ve experienced an injury from smoke inhalation.
- You’re regularly experiencing nausea and/or vomiting.
Here, Dr. Yadegar explains the differences between the different oxygen saturation levels.
Blood oxygen levels chart |
||||
|---|---|---|---|---|
| Range | Blood oxygen level (%) | What it means | ||
| Dangerously low | Below 75% | Seek emergency medical attention immediately–supplementation with oxygen may be necessary. | ||
| Low | Below 90% | Blood oxygen saturation levels below 90% are considered pathological and require evaluation by a healthcare provider. | ||
| Normal | Above 90% | A blood oxygen saturation above 90% is considered clinically normal in patients without any underlying disease. | ||
| High Normal | Mid 90% – 100% | Patients who are healthy often have oxygen saturations in the mid to high 90%. | ||
How to measure blood oxygen levels
To determine if the level of oxygen in your blood is too low, there are two ways to use:
- Take an oxygen level blood draw test, a blood sample to measure your arterial blood gas (ABG)
- Use a pulse oximeter
Oxygen level blood draw test
During an oxygen level blood test, your healthcare provider will take a blood sample from one of your arteries, such as the radial artery found on the inside of your wrist. The blood in arteries has greater levels of oxygen than the blood in veins, making the reading more accurate.
To prepare, your provider may perform an Allen test prior to drawing your blood to make sure you have adequate blood flow. To do this, your provider will place pressure on the radial artery while you’re making a fist. If the color of your skin returns to normal within 5-15 seconds of pressure being released, it’s safe to proceed with the draw.
After a blood sample is drawn, you’ll be asked to apply pressure to the site until bleeding stops. Your results will be available in minutes.
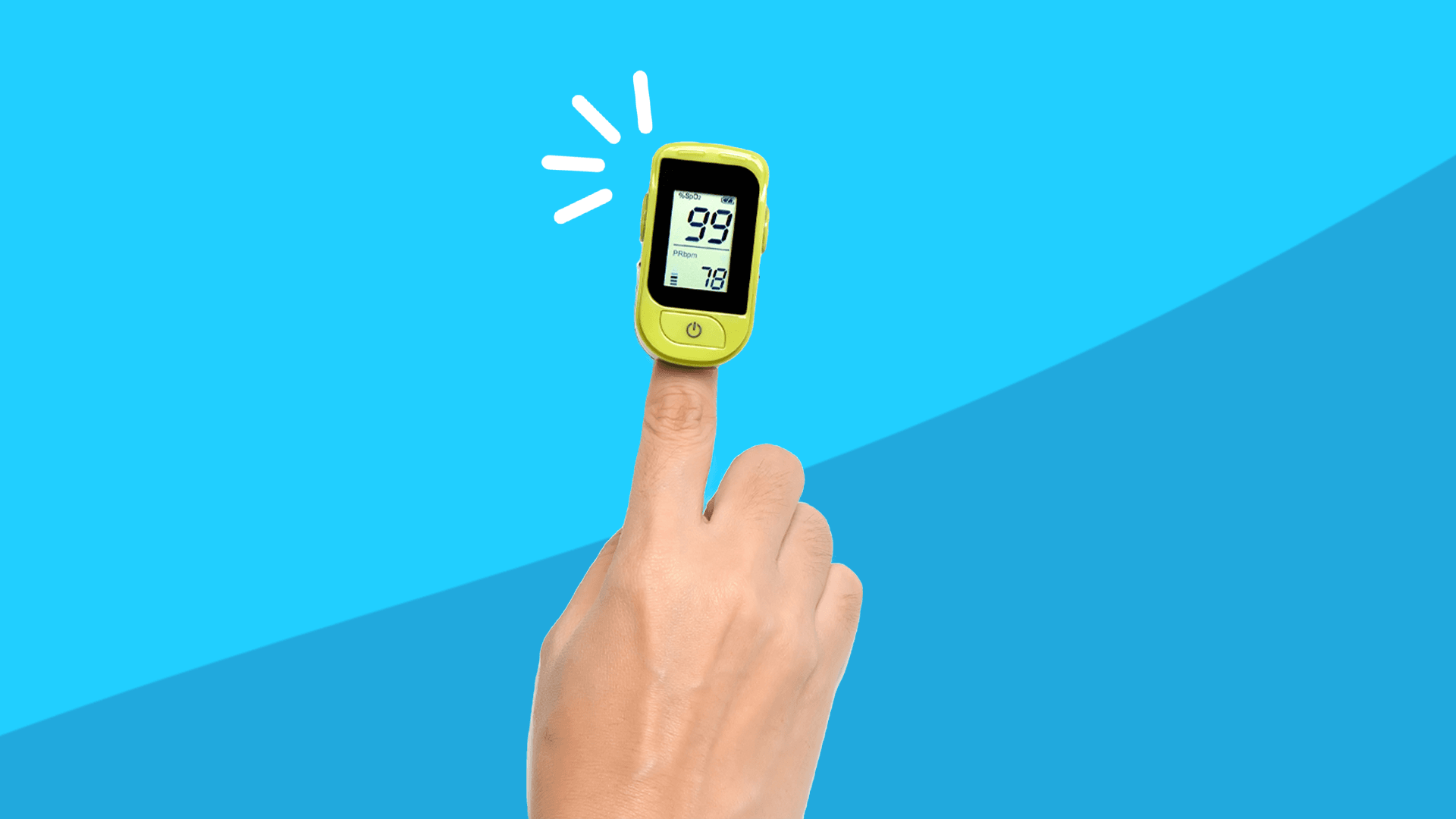
Pulse oximetry
Pulse oximetry measures blood oxygen saturation levels. It is commonly performed in a medical setting such as a doctor’s office or hospital, but you can also measure it at home. This procedure is carried out using a pulse oximeter—a small device you can clip onto a fingertip or other body parts such as your earlobe or toe.
A pulse oximeter works by emitting infrared light into the capillaries of your finger or other body part to measure the amount of oxygen that binds to your red blood cells. The device measures the amount of light reflected off the gasses, determining your oxygen saturation measurement or SpO2 level. In addition, a pulse oximeter can also measure your heart rate.
Although most people will not need to measure oxygen saturation levels, you can do a pulse oximetry test at home. In fact, if your provider has concerns about low oxygen levels, they may ask you to monitor them at home using a pulse oximeter. You can share the readings with your healthcare provider, who can use them to monitor serious lung conditions like chronic obstructive pulmonary disease (COPD), lung disease, or complications from coronavirus. In addition, self-monitoring has become more common during the COVID-19 pandemic.
How accurate are pulse oximeters and what affects their accuracy?
There are different qualities of pulse oximeters, ranging from prescription devices that have received FDA approval to over-the-counter devices that have not been assessed for sensitivity, accuracy, or effectiveness. In fact, some over-the-counter devices may be off by more than six points and the accuracy declines with lower blood oxygen levels. The accuracy of a pulse oximeter may vary depending on the following:
- Poor circulation
- Skin pigmentation
- Skin thickness
- Skin temperature
- Current tobacco (or vaping) use
- Use of fingernail polish
- Movement
- Placement of device (fingers versus toes)
It is important that you do not rely only on a pulse oximeter to assess your health condition or oxygen level. When using pulse oximeter devices, it is recommended you do this in consultation with your healthcare provider. If you are healthy without any significant medical illnesses, it is not necessary to check your pulse oximetry. Doing so may lead to needless worrying.
What causes low blood oxygen levels?
Blood oxygen levels can fluctuate based on several different factors like chronic disease, high altitudes, or illness. Some of the more common risk factors or causes of low blood oxygen levels include:
- Altitude changes, especially high altitude
- Sleep apnea
- Pulmonary fibrosis
- Chronic obstructive pulmonary disease (COPD) such as emphysema, chronic bronchitis
- Asthma
- Carbon monoxide inhalation
- Heart conditions such as congenital heart disease
- Anemia
- Certain medications that depress breathing
- Pulmonary embolism
- Acute respiratory distress syndrome
“Pneumonia is an infection that can also cause inflammation in the air sacs in one or both of your lungs that also results in fluid buildup that eventually can lead to hypoxemia,” says Vivek Cherian, MD, internal medicine physician at Amita Health, an affiliate of Ascension. “If you have pneumonia that is serious enough to cause lower oxygen levels, you typically are admitted to the hospital for close monitoring and treatment.”
COVID-19
If you’ve had COVID-19, your doctor may be treating you for low blood oxygen levels. COVID-19 can trigger a tsunami-like autoimmune proinflammatory response in some patients known as a cytokine storm. In response to certain triggers, including a COVID-19 infection the body can release proinflammatory proteins or “cytokines,” which are tasked to aid the immune system in fighting off foreign pathogens, but instead, attack the patient’s own healthy organs. “These cytokines can damage the vessels within the patient’s lungs, compromising proper gas exchange and causing low blood oxygen saturation, among other serious events,” explains Dr. Yadegar.
Still, research suggests that the occurrence of a cytokine storm is rare, even in COVID-19 patients with respiratory failure. The key to decreasing hospitalization and long-hauler risk is being proactive. “The earlier a patient is found to be developing a COVID-19 related adverse event, the better the prognosis,” Dr. Yadegar says.
Whether you’re in the early stages of a COVID diagnosis or dealing with long-haul symptoms, using a pulse oximeter can help detect potential problems early. But this step is not necessary for everyone. In fact, according to a recent study published in the New England Journal of Medicine, patients in Penn Medicine’s COVID Watch program–designed to keep track of their recovery outside of the hospital using automated text messages–recovered similarly whether or not they used oxygen-measuring devices at home. Your physician can help determine if you are a good candidate for self-monitoring.
RELATED: Compare COVID-19 vaccines
What happens when blood oxygen is too low
While most people show some signs of low blood oxygen levels, some may only know their level is low by taking a pulse oximeter reading or when visiting their healthcare provider. There are some common red flags or symptoms to pay attention to, such as:
- Shortness of breath
- Difficulty breathing
- Bluish color in lips, face, or fingernails
- Chest pain or tightness
- Headache
- Restlessness and discomfort
- A sense of impending doom
- Fast pulse
- Confusion
- High blood pressure (hypertension)
- Cough that gets worse
If you’re experiencing any of the above symptoms of hypoxemia, caused by low levels of oxygen in your blood, consult with a medical provider for diagnosis and treatment options. According to research, acute severe hypoxia can result in loss of consciousness in 10-20 seconds, and permanent brain damage can occur in 3 minutes. Based on its severity and duration, hypoxemia can lead to death, although how low a person’s oxygen level reading can get before becoming fatal varies.
When to contact your healthcare provider
“The most important thing you’d do is to be aware of your symptoms and know when to seek medical help,” Dr. Cherian says. “If you are having persistent fevers or cough, chest pain, coughing up pus, or difficulty breathing, these are all signs you should see a doctor. Also always keep in mind older adults, young children, and people with weakened immune systems are considered to be at high risk, so it’s always important to be vigilant of your symptoms!”
If you’re under the care of a healthcare provider and monitoring levels at home, make sure to note the severity of symptoms. If they are getting worse or blood oxygen levels are lower than 90%, call your provider or 911 right away. For levels above 91% but lower than 94%, call your provider to schedule an appointment. Additionally, if shortness of breath comes on suddenly or interferes with your ability to function—especially if it is accompanied by a fast heart rate, cough, and fluid retention—it’s time to seek emergency care.
How to increase blood oxygen levels
Low blood oxygen level is a serious condition that requires immediate medical attention and treatment. The good news is there are several steps you can take to keep blood oxygen levels in an optimal range.
You’ll first want to establish a baseline blood oxygen level to evaluate for any abnormal decreases. This is the best course of action for patients looking to be proactive in monitoring for serious adverse events.
For patients without any previous chronic pulmonary condition, monitoring blood oxygen saturation at rest and with exertion to evaluate levels below 94% is essential toward promoting better outcomes. Here are some tips that Dr. Yadegar recommends for increasing blood oxygen levels:
- Movement and rest techniques. Walk around your home, and when in bed, lay on your abdomen or side to improve oxygenation. These activities can improve your blood oxygen levels quickly by increasing air flow to the lungs.
- Implement technique breathing known as “4-7-8” breathing. Dr. Yadegar says this breathing technique can help increase lung capacity and reduce stress levels. Inhale for 4 seconds, hold breath for 7 seconds, and exhale for 8 seconds. Just be cautious when attempting deep breathing or heavy exercise outside of your individual baseline, as these can induce further problems including headaches, dizziness, muscle weakness, and fatigue. Doing this or other breathing techniques can increase your blood oxygen level within minutes.
- Quit smoking or vaping. If you smoke, talk to your healthcare provider about quitting. Also, avoid secondhand smoke whenever possible. Two to three weeks after you quit, your circulation will increase, and in 1-9 months, you’ll experience a decrease of shortness of breath–both factors will increase your blood oxygen levels.
- Participate in regular physical activity. Regular exercise such as cardiovascular activities can help boost your overall health. Exercising outdoors while breathing in fresh air can quickly raise your blood oxygen levels.
- Get routine healthcare visits. In addition to regularly meeting with your healthcare provider, you should properly manage medical conditions such as allergic rhinitis, asthma, COPD, sleep apnea, hypertension, or diabetes.
It’s always a good idea to get the green light from your healthcare team before beginning a new routine, or exercise program, especially if you are being treated for low blood oxygen levels.