Key takeaways
TRICARE may cover Wegovy, but it depends on the specific plan and whether you meet all eligibility criteria.
TRICARE typically requires prior authorization and step therapy (trying a cheaper drug first) before covering Wegovy.
Without insurance or discounts, Wegovy costs around $1,844 per month. Insurance can bring that cost down, but most patients still have an out-of-pocket copay.
The good news is that there are ways to save on Wegovy even if your TRICARE plan does not cover it.
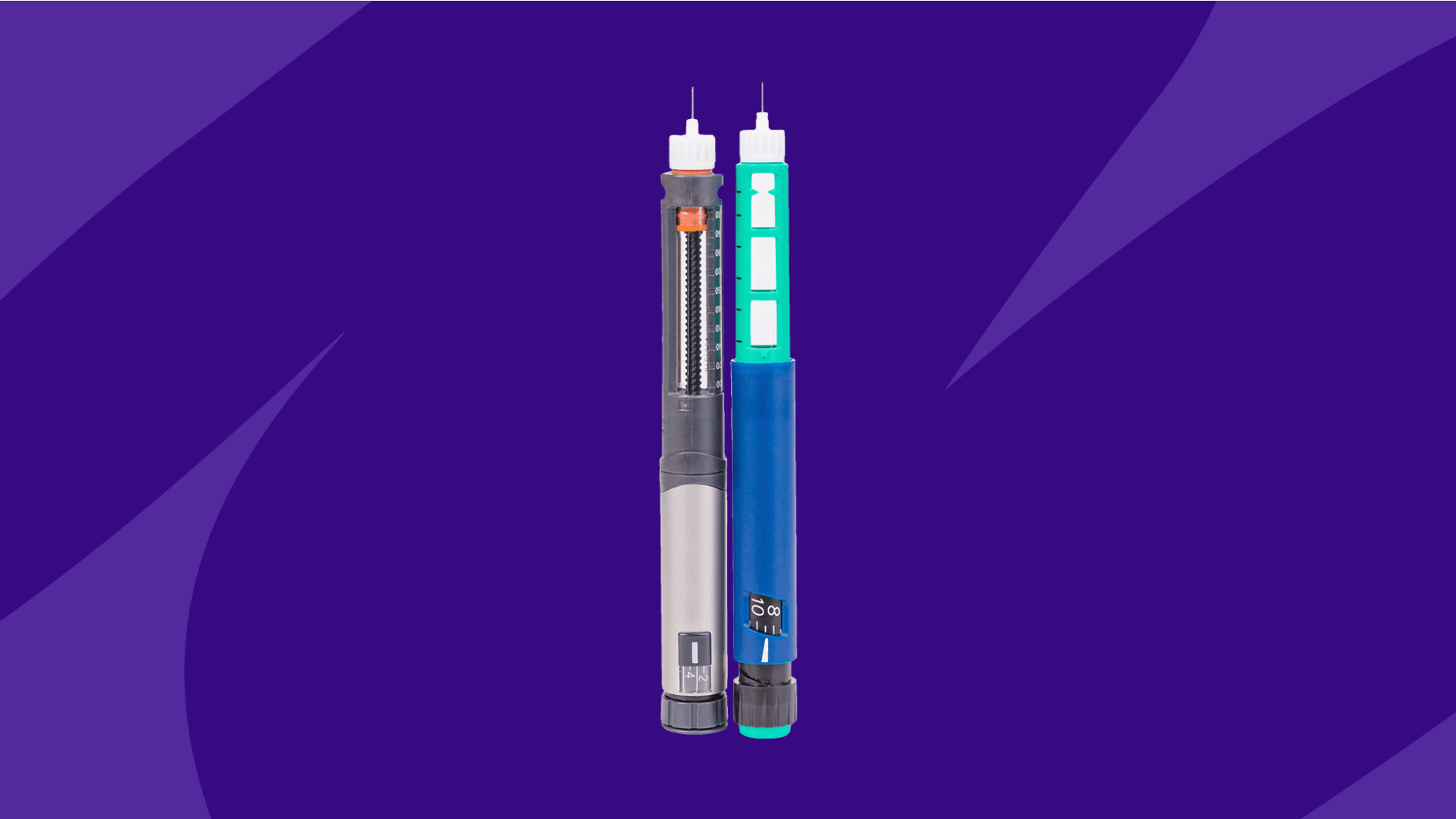
Approximately 4 in 10 U.S. adults have obesity. Treatment typically involves lifestyle changes, but there are also drug treatments like Wegovy (semaglutide), an injectable GLP-1 medication that is FDA-approved for chronic weight management due to its effectiveness in lowering blood sugar and decreasing appetite.
Like most brand-name prescription drugs, Wegovy isn’t cheap. Many patients wonder if health insurance will help offset their out-of-pocket costs. There’s no definitive answer because insurance coverage depends on your specific health plan. Here’s what you should know about Wegovy coverage if you have a policy from TRICARE, the U.S. Department of Defense’s healthcare program for active duty and retiree service members, some National Guard and Reserve members, and their eligible family members.
Save up to 80% on Wegovy with SingleCare Different pharmacies offer different prices for the same medication. SingleCare helps find the best price for you.
Does TRICARE cover Wegovy?
Some — but not all — TRICARE plans cover Wegovy for weight management. According to the TRICARE website, coverage depends on whether your reason for taking Wegovy meets certain criteria and if you have a prescription from a licensed medical provider. TRICARE coverage of Wegovy typically requires prior authorization unless you are also taking other medications for diabetes management.
As of August 31, 2025, several TRICARE plans no longer cover Wegovy or other weight-loss drugs, even if you had an approved prior authorization before. Check the TRICARE formulary to see if Wegovy is covered under your plan.
Reason for taking Wegovy
With the same active ingredient as Ozempic – semaglutide – Wegovy effectively lowers blood sugar. But as Wegovy, insurance plans typically only cover it for weight loss. This brand-name form of semaglutide is not approved for treating diabetes.
However, semaglutide injections, such as Ozempic, are FDA-approved for blood sugar control in Type 2 diabetes. TRICARE is much more likely to cover Ozempic for a person with obesity and Type 2 diabetes, though coverage still depends on the plan.
Getting a prescription from a licensed provider
TRICARE coverage for Wegovy also requires a prescription from a licensed healthcare provider within the TRICARE network.
Michelle Lin, DO, a board-certified doctor of osteopathy at My Family Doc in Las Vegas, Nevada, describes her approach to prescribing obesity drugs: “If the patient is overweight to any degree with failure of diet and exercise, or has the inability to exercise plus metabolic disease, inflammatory musculoskeletal flares, and pain related to carrying more weight, I would consider prescribing Wegovy.”
However, every insurance plan, including TRICARE, has its own criteria for covering weight-loss medications. So while a prescription from a licensed healthcare provider is required, that doesn’t always mean the medication will be covered.
Prior authorization
Finally, TRICARE requires your healthcare provider to complete a prior authorization form for Wegovy. Prior authorization is a process intended to determine a drug’s medical necessity. In the form, your provider must provide reasoning for why Wegovy is necessary. If TRICARE approves the prior authorization, your Wegovy will be covered. If not, you may need to pay for Wegovy out of pocket.
According to the Military Officers Association of America (MOAA), the 2024 TRICARE prior authorization requirements stated that adult patients must meet the following criteria:
- Have a body mass index (BMI) of >30 or a BMI of at least 27 with weight-related risk factors such as high blood pressure or sleep apnea
- Have attempted lifestyle changes, including a reduced-calorie diet, for at least 6 months and still failed to achieve the desired weight loss
- Have tried (or are contraindicated from trying) another prescription weight loss drug. (Requiring patients to try a lower-cost drug before an expensive brand-name medication is known as step therapy.)
- Be committed to lifestyle changes, including a reduced-calorie diet, while on Wegovy
Bottom line: Some TRICARE plans cover Wegovy for eligible enrollees, but there are strict criteria for getting insurance coverage for this particular drug.
How to get approved for Wegovy
If your TRICARE healthcare plan does not initially cover Wegovy, you still have a few options for getting approved.
- Send an appeal letter to TRICARE. You can talk to your healthcare provider about ways to state that the drug is medically necessary. Novo Nordisk offers a sample letter that some healthcare providers use as a template. Even if your provider offers to write an appeal letter, you might need to submit the letter to TRICARE yourself.
- Enroll in a clinical trial. If TRICARE will not cover Wegovy for you, consider enrolling in a clinical trial for Wegovy. If you qualify for a plan currently enrolling trial participants, you can get Wegovy for free or at a steeply discounted price.
- Switch to a different weight-loss drug. Saxenda and Zepbound are two Wegovy alternatives that might be covered by insurance. Other GLP-1s like Ozempic and Mounjaro are sometimes prescribed off-label for weight loss, though off-label prescriptions are unlikely to be covered by insurance. Some TRICARE plans do not cover weight-loss drugs.
How much does Wegovy cost?
Wegovy is a costly weight-loss medication. The average retail cost is $1,844 per four injection pen, which is a one-month supply. For people with insurance coverage, the out-of-pocket copay for Wegovy varies by plan.
How to check whether your TRICARE plan covers Wegovy
You can check your insurance coverage with this web tool from Novo Nordisk, Wegovy’s manufacturer. You can also use the TRICARE formulary search tool to view the TRICARE formulary (list of covered drugs).
That said, the best way to get a definitive answer about drug coverage is to contact your TRICARE representative. In most cases, you can call the number on the back of your insurance card or prescription card.
How to save on Wegovy
There are ways to save on Wegovy even if your insurance plan does not cover it. For instance, cash payers can use a SingleCare prescription discount card or a SingleCare coupon to save over $600 per month on the retail price of Wegovy. Simply click “Get free coupon” to have the coupon texted or emailed to you. Then, take it to a participating pharmacy to fill your Wegovy prescription.
- TRICARE eligibility, Military Benefit Association
- FDA approves new drug treatment for chronic weight management, first since 2014 U.S. Food & Drug Administration (2021)
- FAQs, TRICARE (Updated 8/4/2025)
- Weight Loss Products, TRICARE (Updated 8/26/2025)
- MOAAS TRICARE guide: Weight loss drugs and TRICARE, Military Officers Association of America (2024)
- Enrolling in a clinical trial for Wegovy, Clinicaltrials.gov