Compare furosemide alternatives | Bumetanide | Chlorthalidone | Spironolactone | Valsartan | Lisinopril | Natural alternatives | How to switch meds
Furosemide (brand name Lasix) is a common medication used to treat fluid retention (edema) due to pulmonary edema, congestive heart failure, cirrhosis of the liver, or renal failure. This prescription medication can also be used to lower blood pressure in people with high blood pressure (hypertension). Typically furosemide is used along with other medications to lower blood pressure. Furosemide belongs to the class of medications called loop diuretics and are often referred to as “water pills”. Loops diuretics work to increase the body’s elimination of water and salt that leads to a reduction in excess fluids from the body’s tissues and lower blood pressure. Furosemide is available as an oral tablet and oral solution and may be prescribed for either short-term or long-term treatment of edema.
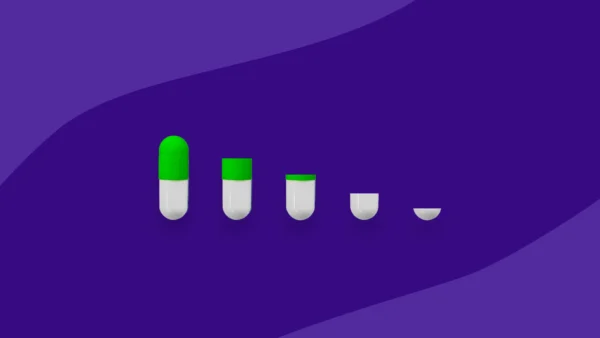
While an effective treatment for some people, furosemide may not be the best and safest option for all people managing fluid retention or high blood pressure. Diuretics like furosemide have common side effects of dehydration and electrolyte imbalances. These effects are more common with higher doses and a restricted salt intake. People using furosemide are monitored for signs of fluid or electrolyte imbalance such as low potassium, sodium, magnesium, and calcium levels in the blood. Symptoms of dehydration and electrolyte imbalances include dry mouth, thirst, weakness, lethargy, drowsiness, restlessness, muscle pains or cramps, muscular fatigue, hypotension, low urine output, fast heart rate, irregular heartbeat, or gastrointestinal disturbances such as nausea and vomiting. An alternative to furosemide may be considered for certain individuals such as elderly people or those who have difficulty with urination.
RELATED: Lasix side effects and how to avoid them
What can I take in place of furosemide?
There are other options available to treat fluid retention and high blood pressure that do not improve with furosemide. When considering alternative prescription medication, it’s important to consider the specific condition being treated. Depending on the reason furosemide is being prescribed, there are several classes of medications that could be used as alternatives including other loop diuretics, thiazide diuretics, potassium-sparing diuretics, angiotensin II receptor blockers (ARBs), angiotensin-converting enzyme (ACE) inhibitors, calcium-channel blockers (CCBs), beta blockers, alpha blockers, and central alpha agonists. These treatment options may be more suitable for certain individuals due to their different uses, side effect profiles, and dosages.
Compare furosemide alternatives |
|||
|---|---|---|---|
| Drug name | Uses | Dosage | Coupons |
| Lasix
(furosemide) |
|
|
Lasix coupons |
| Bumex
(bumetanide) |
Edema | 0.5 to 10 mg per day by mouth divided into one to two doses | Bumex coupons |
| Demadex (torsemide) |
|
|
Demadex coupons |
| Diuril (chlorothiazide) |
|
|
Diuril coupons |
| Microzide
(hydrochlorothiazide) |
|
|
Microzide coupons |
| Thialitone
(chlorthalidone) |
|
|
Thialitone coupons |
| Aldactone
(spironolactone) |
|
|
Aldactone coupons |
| Dyrenium
(triamterene) |
Edema | 100 mg tablet by mouth twice daily | Dyrenium coupons |
| Cozaar
(losartan) |
|
50 to 100 mg tablet by mouth once daily | Cozar coupons
|
| Diovan
(valsartan) |
|
|
Diovan coupons |
| Zestril
(lisinopril) |
|
10 to 40 mg tablet by mouth once daily | Zestril coupons
|
| Vasotec
(enalapril) |
|
5 to 40 mg per day by mouth divided into one to two doses | Vasotec coupons |
Other alternatives to furosemide
Depending on the reason furosemide is being prescribed, there are several classes of medications that could be used as alternatives.
Angiotensin II receptor blockers (ARBs)
- Edarbi (azilsartan)
- Atacand (candesartan)
- Teveten (eprosartan)
- Avapro (irbesartan)
- Benicar (olmesartan)
- Micardis (telmisartan)
Angiotensin-converting enzyme (ACE) inhibitors
- Lotensin (benazepril)
- Capoten (captopril)
- Monopril (fosinopril)
- Univasc (moexipril)
- Aceon (perindopril)
- Accupril (quinapril)
- Altace (ramipril)
- Mavik (trandolapril)
Calcium-channel blockers (CCBs)
- Norvasc (amlodipine)
- Cardiazem (diltiazem)
- Plendil (felodipine)
- Cardene (nicardipine)
- Procardia (nifedipine)
- Sular (nisoldipine)
- Verelan (verapamil)
Diuretics
- Inspra (eplerenone)
- Lozol (indapamide)
- Zaroxolyn (metolazone)
Beta blockers
- Sectral (acebutolol)
- Tenormin (atenolol)
- Kerlone (betaxolol)
- Zebeta (bisoprolol fumarate)
- Coreg (carvedilol)
- Trandate, Normodyne (labetalol)
- Toprol XL (metoprolol succinate)
- Lopressor (metoprolol tartrate)
- Corgard (nadolol)
- Bystolic (nebivolol)
- Visken (pindolol)
- Inderal (propranolol)
- Betapace (sotalol)
Alpha blockers
Central alpha agonists
- Catapres (clonidine)
- Tenex (guanfacine)
- Aldomet (methyldopa)
Top 5 furosemide alternatives
The following are some of the most common alternatives to furosemide.
1. Bumetanide (Bumex)
Bumetanide is a loop diuretic used to treat edema associated with congestive heart failure, liver disease, and kidney problems . As a similar medication to furosemide, bumetanide may also be used to help lower blood pressure. The loop diuretics torsemide and bumetanide have an oral bioavailability (the fraction of drug that reaches systemic circulation) of 80 to 100%, while furosemide has a wide variant bioavailability of 10 to 100%. In patients with chronic renal insufficiency, furosemide has been shown to have a variable dose response compared with a more consistent dose effect with bumetanide due to altered metabolism of furosemide in patients with kidney disease. Switching to bumetanide may be a suitable option for people who have become resistant to furosemide or those with concerns regarding bioavailability. Bumetanide is dosed as 0.5 to 10 mg per day by mouth divided into one to two doses.
RELATED: Bumex vs. Lasix: Differences, similarities, and which is better for you
2. Chlorthalidone (Thalitone, Hygroton)
Chlorthalidone also works as a water pill in the group of medications called thiazide diuretics. Unlike furosemide, chlorthalidone is recommended as a first-line medication for treating hypertension according to the American Heart Association (AHA) hypertension guidelines. Aside from hypertension treatment, chlorthalidone can be used to treat edema and decrease swelling of fluid trapped in the body’s tissues. Chlorthalidone may be considered as an alternative for people needing further improvement in the management of hypertension. Like furosemide, it’s important to have fluid status and electrolytes monitored. Chlorthalidone is dosed as a 12.5 to 25 mg tablet by mouth once daily for hypertension and a 50 to 100 mg tablet by mouth once daily for edema.
3. Spironolactone (Aldactone)
Spironolactone works as a different type of diuretic called an aldosterone antagonist. Spironolactone is used to manage heart failure, hypertension, edema associated with hepatic cirrhosis or nephrotic syndrome, and primary hyperaldosteronism. Possible side effects of spironolactone include breast enlargement or swelling (gynecomastia), elevated potassium levels in the blood (hyperkalemia), decreased sexual drive, menstrual irregularities, dehydration, electrolyte disturbances, dizziness, and muscle cramps. Spironolactone may be best suited for those also managing hyperaldosteronism, a condition in which one or both adrenal glands produce too much of the hormone aldosterone potentially leading to lower potassium levels, weakness, and muscle spasms.
RELATED: Spironolactone side effects and how to avoid them
4. Valsartan (Diovan)
Valsartan works as an angiotensin II receptor blocker (ARB). According to the American Heart Association (AHA) hypertension guidelines, ARBs like valsartan are first-line treatment options for managing hypertension. Valsartan has additional FDA indications including heart failure and post-myocardial infarction (after a heart attack). Valsartan may be considered as an alternative for people managing hypertension and heart failure. In The Valsartan Heart Failure Trial (Val-HeFT), valsartan significantly reduced hospitalizations for heart failure. Valsartan is either dosed as a 80 to 320 mg tablet by mouth once daily for hypertension or as a 160 mg tablet by mouth twice daily for heart failure or post-myocardial infarction.
5. Lisinopril (Zestril)
Lisinopril works as an angiotensin-converting enzyme (ACE) inhibitor. Lisinopril is recommended as a first-line medication for treating hypertension according to the AHA hypertension guidelines. Aside from treatment of hypertension, lisinopril has other FDA indications including heart failure and reduction of mortality in acute myocardial infarction (heart attack). Lisinopril and other ACE inhibitors should not be used in pregnant women due to fetal toxicity risk. ACE inhibitors have potential for a unique adverse effect of persistent cough. The cough can be bothersome to some people and require a change in medication. Lisinopril is dosed as a 10 to 40 mg tablet by mouth once daily.
Natural alternatives to furosemide
Alternative remedies for furosemide include lifestyle changes and diet modifications to help keep blood pressure in a healthy range or to decrease edema. According to the American Heart Association (AHA) hypertension guidelines, alternative remedies are effective at lowering blood pressure and benefiting heart health.
Lifestyle modifications include regular physical exercise, weight loss, and diet changes. Being overweight, especially weight in the belly, is linked to increased blood pressure, according to the American College of Cardiology. A heart-healthy diet, such as the DASH (Dietary Approaches to Stop Hypertension) diet, is recommended for people with hypertension. The DASH diet focuses on eating fruits, vegetables, low fat milk, whole grains, fish, poultry, beans, and nuts. This diet also aims to decrease sodium, foods and beverages with added sugars, and red meat. Additionally, the AHA recommends adults with elevated blood pressure or hypertension who currently consume alcohol should limit their intake to no more than 2 standard drinks for men and 1 standard drink for women per day.
Some foods have diuretic effects that can help people reduce water retention and swelling. Watermelon has been found to have diuretic activity which may be attributed to increase in salt excretion ability. Other fruits such as oranges, lemons, and limes can get rid of excess fluid. These fruits contain minerals and enzymes that cause water release from the kidneys.
How to switch to a furosemide alternative
1. Discuss all health conditions with a healthcare provider
Before switching from furosemide to an alternative, it’s important that the prescribing doctor is aware of all medical conditions. Some alternatives should be used with caution or avoided with certain medical conditions. For example, all medications that contain ACE inhibitors (such as lisinopril and enalapril) and ARBs (such as valsartan and losartan) must not be used in pregnant women or women planning on becoming pregnant. Alternatives in the beta blocker antihypertensive class (such as atenolol and metoprolol succinate) must be avoided in certain heart conditions such as bradycardia (slow heart rate). If cost is a concern for switching medications, SingleCare can help with savings on prescription costs at local pharmacies nationwide.
2. Do not suddenly stop taking furosemide without medical advice
Only stop taking furosemide if the prescribing doctor has been consulted and decided stopping the medication is safe. If furosemide is stopped suddenly, there might be a sudden spike in blood pressure or increase in swelling. Diuretics affect the body’s regulation of urination (diuresis), water volume, and salt concentration. When furosemide wears off, the body may overcompensate by retaining too much sodium chloride and fluids, causing fluid build-up or high blood pressure. Too much fluid in the body could become life threatening. In people with serious health conditions, such as congestive heart failure, diuretic withdrawal may require monitoring. It’s important for a therapy plan to be established prior to stopping furosemide suddenly.
3. Discuss all prescription and over-the-counter medications with a healthcare provider
Before switching from furosemide to an alternative, it’s important that the prescribing doctor has reviewed a patient’s medication list including prescription drugs, over-the-counter medications, and supplements. Some alternatives have dangerous drug interactions that must be avoided.
4. Continue to monitor blood pressure readings
For those managing hypertension, it’s important to check blood pressure with an at home monitor. Keeping a blood pressure journal can help healthcare providers determine if the medication plan is working or not.
5. Watch for signs of dehydration or electrolyte imbalance
Diuretics can cause dehydration and electrolyte imbalance. It’s important to watch for signs of severe dehydration or electrolyte depletion such as dry mouth, dry eyes, muscle cramps, drowsiness, fatigue, weakness, irregular heartbeat, or fast heartbeat. The amount of fluid intake and the types of fluid consumed may be restricted for certain people managing conditions with diuretics. If fluids are not restricted, immediately take fluids at signs of dehydration. If fluids are restricted, call a healthcare provider for medical advice.
Use extra caution on hot summer days, as people are more likely to get dehydrated and lose electrolytes. People can either avoid or limit their time spent outdoors on hot days and always carry a water bottle.