What are the early signs of psoriasis?
Overview: What does psoriasis feel/look like?
Psoriasis is a chronic autoimmune skin disease that causes skin swelling, discoloration, and the rapid growth of skin cells. Psoriasis can also affect the joints and eyes. The most common signs of psoriasis are swollen, red, and silvery patches on the skin that are commonly well-defined. They can occur anywhere on the body but most commonly appear on the arms, legs, midsection, lower back, and scalp. These skin eruptions are often itchy and sometimes painful. The affected skin areas can look different depending on the type of psoriasis, as some may be round, scaly, or oval patches while others may be non-infectious pus-filled bumps. According to the National Psoriasis Foundation, the five types of psoriasis are plaque, guttate, inverse, erythrodermic, and pustular psoriasis. The patches can affect small areas of the skin or, in some people, most of the body. Psoriasis can also affect the nails, the mouth, the eyes, or the joints.
Key takeaways:
Psoriasis is a common health condition that primarily affects adults but can affect anyone regardless of age, sex, race, or ethnicity.
Early signs of psoriasis include the development of small, discolored bumps on the skin that join together into a larger, thickened, scaly area of skin.
Serious symptoms of psoriasis, such as large areas of skin affected by rash, pustules, or plaques, along with fever, chills, muscle weakness, and fatigue, may require immediate medical attention.
The immune system and environmental triggers cause psoriasis. You may be at risk for developing psoriasis symptoms if you have an immediate relative with psoriasis. Other risk factors include smoking, obesity, and alcohol abuse.
People can develop psoriasis at any age, but developing it is most common between 20 and 30 years old and between 50 and 60 years old.
Psoriasis usually requires a medical diagnosis.
Psoriasis generally requires treatment. Psoriasis symptoms typically improve with treatment.
Treatment of psoriasis may include oral, injected, or topical drugs that reduce swelling, suppress the immune system, or provide relief of symptoms. Other treatment options include phototherapy, lifestyle changes, and avoiding triggers. Read more about psoriasis treatments here.
People with psoriasis have a greater chance of having complications like reduced quality of life, depression, infections, psoriatic arthritis, lymphoma, skin cancer, Crohn’s disease, ulcerative colitis, metabolic syndrome, and heart attack.
Use coupons for Humira (adalimumab), Otezla (apremilast), and Tazorac (tazarotene) to save up to 80%.
What are the early signs of psoriasis?
The earliest sign of psoriasis is likely an initial flare-up on some part of the skin. A psoriasis flare-up typically starts as small, discolored bumps on the skin. White scales form on the outside, and the bumps can join and form a more extensive, discolored, scaly area on the skin.
Other psoriasis symptoms
In most people, psoriasis affects the skin but can cause other symptoms. A psoriasis flare-up typically starts with small skin bumps or a rash. Signs of a psoriasis flare-up may have several manifestations, depending on the type of psoriasis:
Skin patches that are raised, discolored, and covered with silvery scales that easily come off or shed
A rash of small red patches
Skin patches that are red but without the scales
Skin patches covered in pus-filled bumps, usually on the hands or feet
Skin discoloration and swelling on most or all of the body
These patches may be itchy or painful. If most of the skin surface is affected, the affected areas can be severely painful or burning
Other symptoms might include:
Cracking of the skin
Dry skin
Pitting, cracking, or crumbling of fingernails or toenails
Furrows or grooves on the tongue
Psoriatic arthritis is diagnosed when psoriasis flare-ups attack the joints, affecting both small and large joints, and commonly in the fingers and toes. Symptoms of psoriatic arthritis include:
Joint swelling and pain
Swollen fingers and toes (“sausage fingers”)
Joint stiffness
Reduced range of joint motion
Psoriasis can also affect the eye, causing symptoms such as:
Swollen eyelids
Drooping eyelid
Loss of eyelashes
Eye redness
Eye pain
Vision changes
Psoriasis vs. eczema symptoms
Eczema is a common skin condition that can look a lot like psoriasis. Similar to psoriasis, eczema can make the skin dry, red, itchy, or scaly. Some outbreaks are caused by allergies, but other types may be due to stress, anxiety, depression, or an infection. Though aggravating, eczema is not a health-threatening condition. Psoriasis, on the other hand, is a chronic and potentially severe problem that requires medical treatment. Knowing the difference can help forestall many of the long-term problems associated with psoriasis.
| Psoriasis | Eczema | |
| Shared symptoms |
|
|
| Unique symptoms |
|
|
RELATED: Is it just dry skin? Or could it be eczema? Or psoriasis?
Types of psoriasis: How can I tell which one I have?
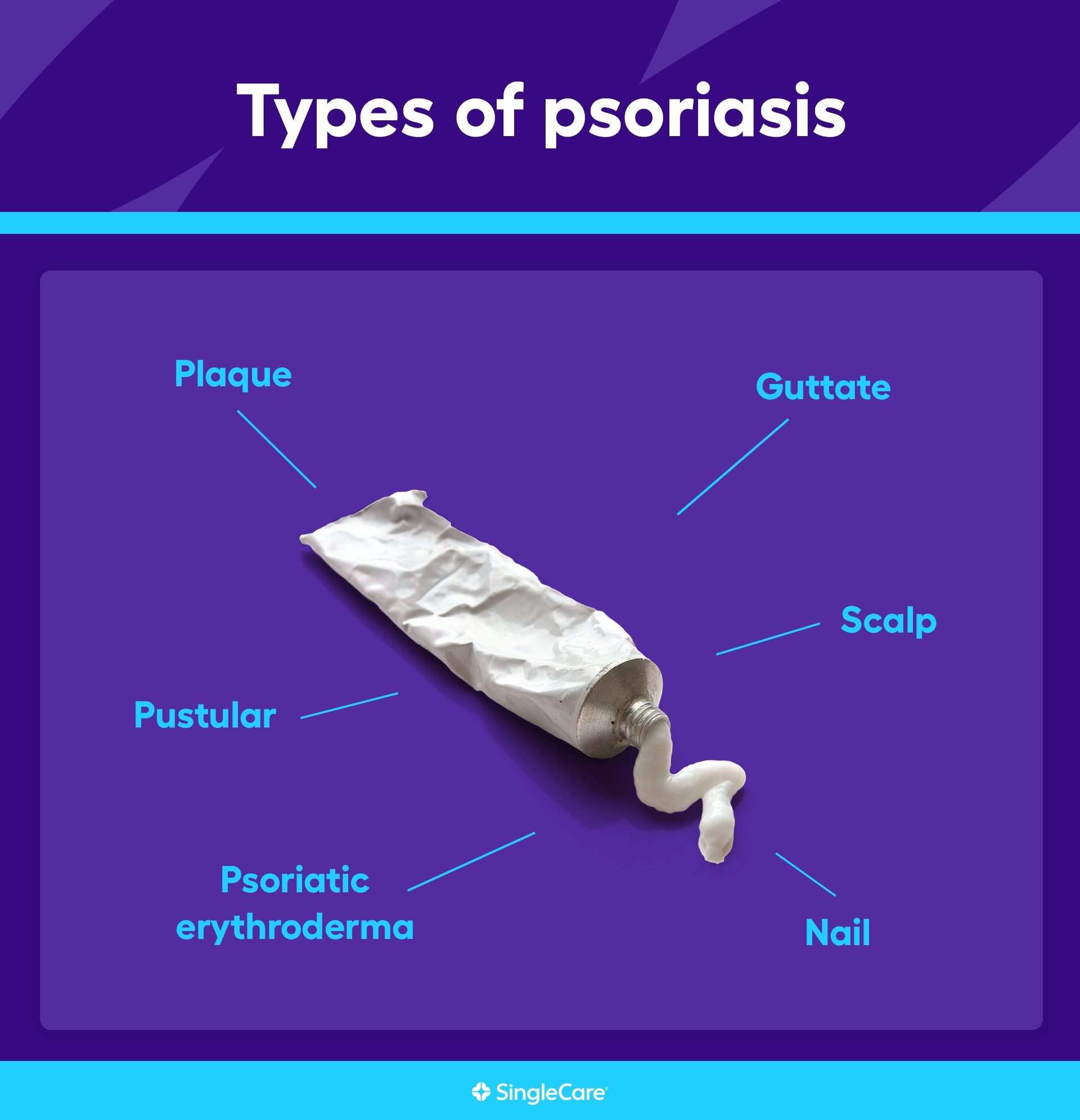
Psoriasis is diagnosed primarily based on how flare-ups manifest on the skin:
Plaque psoriasis, the most common type of psoriasis, is characterized by thick, raised, discolored, and scaly patches of skin that usually form on the legs, arms, trunk, or scalp
Inverse psoriasis typically causes unraised red patches in the skin folds such as the armpits, inner elbows, backs of the knees, genitals, between the buttocks, or in the breast folds
Guttate psoriasis primarily affects children and young adults—often after a strep throat infection—and is characterized by a rash of small, discolored spots with only slight flaking that primarily appears on the midsection
Erythrodermic psoriasis is a rare, severe, and potentially life-threatening type of psoriasis where lesions cover most or all the skin on the body and cause extreme pain—other symptoms include fever, chills, weakness, and rapid heartbeat
Pustular psoriasis is an uncommon form of psoriasis that affects the hands and feet and is characterized by red, swollen, and painful skin patches covered with non-infectious pus-filled bumps
Generalized pustular psoriasis, or von Zumbusch psoriasis, is a very rare, severe, and potentially life-threatening type of psoriasis characterized by pus-filled bumps, erupting all over the body along with headache, fever, weakness, and several other symptoms
In addition, healthcare professionals often distinguish between types of psoriasis based on the part of the body affected. They aren’t any different from the types of psoriasis listed above, but they are important in making treatment decisions:
Nail psoriasis is any case in which the fingernails and toenails are affected and become pitted, cracked, discolored, detached, or crumble away
Scalp psoriasis is any case of plaque psoriasis on the scalp and is characterized by patches of discolored, raised, and scaly patches that are also greasy
Oral psoriasis describes any case where the mouth is affected, causing fissures on the top of the tongue, redness in the mouth, and mouth sores
Psoriatic arthritis involves any case in which the joints are affected—about 20% of people with psoriasis will develop psoriatic arthritis
When to see a doctor for psoriasis symptoms
See a healthcare provider if any of the symptoms of psoriasis are noticed. The problem can get worse, so treatment should begin as early as possible. If the symptoms are very severe and affect large areas of the body, then emergency treatment is required. There will typically be other symptoms such as fever, chills, racing heartbeats, weakness, and extreme pain. These severe cases can have potentially life-threatening complications.
For most people, the final diagnosis and treatment plan requires the services of a dermatologist. The diagnosis will involve a medical history and a physical examination of the affected skin. Standard blood tests may be ordered as a routine check. In many cases, that’s all that’s needed for a diagnosis.
In more doubtful cases, the healthcare provider may take a scraping or sample of the affected skin to study under a microscope, a procedure called a biopsy. A blood test may be used to check for potential indicators of a psoriasis flare-up or to rule out other health problems.
Complications of psoriasis
Complications of psoriasis include:
Reduced quality of life
Poor self-image
Depression
Psoriatic arthritis
Increased risk of heart attack
Increased risk of lymphoma
Increased risk of metabolic syndrome
Increased risk of Crohn’s disease
How to treat psoriasis symptoms
During an active flare-up, both topical and oral medications can help relieve symptoms. Doctors may prescribe medications to prevent psoriasis in people with moderate to severe psoriasis flare-ups. These drugs block the immune system and are taken continuously, not just during an attack. Medications include:
Topical corticosteroids to reduce swelling
Topical and oral retinoids (drugs similar to vitamin A) to slow down skin growth and reduce swelling
Topical vitamin D analogs to reduce scaling and inflammation
Zithranol (anthralin) to reduce swelling and slow down skin growth
Topical calcineurin inhibitors to block the immune system at the affected area
Oral calcineurin inhibitors that block the immune system throughout the body are used to treat severe psoriasis outbreaks
The PDE4 inhibitor Otezla (apremilast) is an oral medication used to reduce inflammation
Topical salicylic acid to soften and remove scales
Oral or injectable methotrexate
Biologic medications such as Cosentyx (secukinumab), Humira (adalimumab), Stelara (ustekinumab)
Other treatments include:
Phototherapy (or light therapy), in which affected areas are exposed to ultraviolet light to slow the rate of skin growth and reduce inflammation
RELATED: Everything you need to know about biologics for psoriasis
Living with psoriasis
Psoriasis is a chronic, lifelong condition. That means living with psoriasis is a lifelong project. Here are some tips for managing psoriasis:
Take all medications as instructed
Because psoriasis can change over time, make sure to keep regular appointments with all members of the care team
Because of the increased risk for other illnesses such as heart disease, get regular checkups
Keep a symptom diary that tracks symptoms, duration of symptoms, possible triggers, and medication side effects
Avoid common triggers such as stress or sunburn
Avoid drugs that might trigger an attack such as NSAIDs, beta blockers, or lithium
Once you’ve recognized your own triggers, avoid them
Protect yourself from skin injuries
Tell the primary healthcare provider about mood changes such as depression or anxiety
Lose weight
Reduce alcohol intake
Quit smoking
Reduce stress
Join a support group
Most importantly, see a doctor
If there’s any suspicion that a skin problem might be psoriasis, see a healthcare provider. A psoriasis diagnosis, though unwelcome, is not necessarily a cause for distress. About 75% of psoriasis cases are mild. Although there is no cure, treatments like steroid creams can effectively manage symptoms and improve quality of life.
FAQs about psoriasis symptoms
Can psoriasis make you feel sick?
Severe psoriasis that affects most of the body’s skin can cause fever, chills, muscle weakness, headache, and feeling sick.
Does psoriasis make you gain weight?
Psoriasis does not cause weight gain, but people with psoriasis are at greater risk for developing metabolic syndrome, a constellation of medical conditions that are often associated with obesity.
Can psoriasis symptoms be mistaken for shingles?
Although both psoriasis and shingles can cause bad rashes on the skin that may burn or itch, shingles are painful, sometimes extremely painful. Shingles typically only develop on one side of the body. The pain typically starts before any rash appears and often continues for months or even years after the rash disappears. Shingles can also cause severe illness, with symptoms such as fever, fatigue, and headache.
What’s next? Additional resources for people with psoriasis symptoms
Test and diagnostics
Psoriasis, American Family Physician
Psoriasis, StatPearls
Psoriasis beyond the skin: ophthalmological changes (review), Experimental and Therapeutic Medicine
Psoriasis: signs and symptoms, American Academy of Dermatology Association (AAD)
Treatments
Everything you need to know about biologics for psoriasis, SingleCare
Phototherapy, National Psoriasis Foundation
Psoriasis, StatPearls
Psoriasis treatments and medications, SingleCare
Scientific studies and clinical trials
Reasons for hospitalization of psoriasis patients a report from the National Inpatient Sample, Cureus
More information on related health conditions
Eczema, Cleveland Health Clinic
Eczema treatments and medications, SingleCare
Is it just dry skin? Or could it be eczema? Or psoriasis?, SingleCare
Psoriasis or eczema?, National Psoriasis Foundation
Stephanie Melby, B.S., Pharm.D., received a bachelor of science in nutrition from the University of Minnesota and a doctorate of pharmacy from the University of New England. She has seven years of experience in retail pharmacy and is certified in Medication Therapy Management (MTM). Dr. Melby resides in Minneapolis, Minnesota.
...Related Drugs
Related Drug Information
- What is Sandimmune
- What is Gengraf
- What is Methotrexate (Anti-Rheumatic)
- Otezla dosage, forms, and strengths
- What is Otezla
- What is Zithranol
- What is Differin
- What is Tretinoin
- Methotrexate dosage, forms, and strengths
- Humira dosage, forms, and strengths
- What is Humira
- What is Zithranol
- What is Tazorac
- What is Topicort
- What is Retin-A
Popular Prescriptions
Subscribe to our savings newsletter
Health education, drug info, wellness & more
SingleCare is a prescription discount service that offers free coupons on thousands of prescription drugs. It can be used whether you have insurance, Medicare, Medicaid, or none of the above, but it cannot be combined with insurance.
SingleCare provides transparent drug pricing, so you can compare discounts at pharmacies near you. Browse singlecare.com to find drug discounts, helpful information about your prescription, and resources to help you make informed health decisions.
Prescription savings vary by prescription and by pharmacy, and may reach up to 80% off cash price. This is a medical discount plan. This is NOT insurance. This program offers you the opportunity to locate providers of various types of medical services who will offer their services to you at discounted rates. The range of discounts for medical or ancillary services provided under the plan will vary depending on the type of provider and service received. You are fully responsible for paying for all health care services but will be entitled to receive a discount from those health care providers in accordance with the specific pre-negotiated discounted fee schedule. This program does not guarantee the quality of the services or procedures offered by the providers. Except for prescription drugs which you will pay directly to the pharmacy at the time of purchase, all other services received through a program provider will be charged to the credit card on file in your member account. The charge will include an administrative fee for use of the program. Towers Administrators LLC is the licensed discount medical plan organization with its administrative office located at 4510 Cox Road, Suite 111, Glen Allen, VA 23060. SingleCare Services, LLC is the marketer of the discount medical plan organization including its website, singlecare.com, with its corporate office located at 99 High Street, Suite 2800, Boston, MA 02110. For additional information, including an up-to-date list of providers, or assistance with any issue related to program membership, please contact member support any time at www.singlecare.com, or by calling toll-free 844-234-3057, 24 hours, 7 days a week (except major holidays). Pharmacy names, logos, brands, and other trademarks are the property of their respective owners.
Blog articles are not medical advice. They are intended for general informational purposes and are not meant to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. If you think you may have a medical emergency, immediately call your physician or dial 911.
© 2026 SingleCare Administrators. All rights reserved
© 2026 SingleCare Administrators. All rights reserved







