Key takeaways
Nearly 40% of Americans taking prescription medications are unaware of potential interactions with vitamins and supplements, posing risks to their health.
For example, supplements like St. John’s wort can diminish the effectiveness of SSRIs and birth control.
Consult healthcare providers before combining supplements with medications.
Adding vitamins and supplements to your daily care regimen can help improve your general health and stave off ailments. However, many don’t realize that certain vitamins and supplements can also affect prescription medications when mixed. According to a national Wakefield Research survey, nearly 40% of Americans who take prescription medications are unaware of vitamin interactions.
RELATED: See our best supplement prices
Can you take medicine and vitamins together?
When it comes to supplements, you may think that because they’re natural, they’re safe, but that’s not necessarily true. Companies that produce vitamin supplements are not required to get approval from the Food and Drug Administration before selling their products, so it can be hard to determine whether they are safe or effective—even if they contain the exact ingredients listed. And it can be risky to take certain supplements with prescription medications.
Although the FDA requires all supplements to be labeled correctly, not all companies follow these guidelines or report the amounts contained accurately. What’s more, the majority of these supplements lack scientific evidence to support their claims to foster good health. Before you start taking any vitamins or supplements, discuss their safety and possible drug interactions with your healthcare provider or pharmacist. And remember, your best bet to get the required vitamins and minerals is eating a well-rounded, healthy diet. These are a few examples of how supplements and medications can negatively impact one another.
Vitamin interactions with antidepressants
The combination of SSRI antidepressant medications with supplements can be especially dangerous. If you have an anxiety disorder or depression, your healthcare provider may prescribe a selective serotonin reuptake inhibitor (SSRI). Common SSRIs are Lexapro, Prozac, Paxil, and Zoloft. These are safe for most people, but when taken with certain supplements or vitamins, the results can be risky. Brandi Cole, Pharm.D., a medical advisory board member for Persona Nutrition, explains what supplements you can’t take with SSRIs, and why.
- St. John’s Wort may decrease a medication’s effectiveness: “Most SSRIs are extensively metabolized by liver enzymes, and supplements that affect these enzymes could potentially change the way your body eliminates SSRIs,” Cole says. “For example; St. John’s wort induces liver enzymes—meaning it makes the liver eliminate certain prescription drugs more quickly than normal.” Translation: St. John’s wort causes your system to clear SSRIs sooner than intended, and without the correct amount of medication in your system, your medication can’t work as well.
- 5HTP (5-hydroxytryptophan) can increase the risk of serotonin syndrome: Supplements that contain serotonin or alter serotonin metabolism—such as 5HTP (a serotonin precursor), SAMe, or St. John’s wort can cause (the potentially life-threatening) serotonin syndrome when taken with SSRIs.
You may be wondering if you can take multivitamins with antidepressants. While multivitamins may seem like a safe bet, it’s best to consult with your healthcare provider to find out before you start taking any vitamin, mineral, or herbal supplements.
Lexapro coupons | Prozac coupons | Paxil coupons | Zoloft coupons
Vitamin interactions with birth control
But it’s not just SSRIs. If you are a woman who uses oral contraceptives for birth control, beware of St. John’s wort. “St. John’s wort can render contraceptives useless if you’re taking it regularly,” Cole says. “In fact, taking St. John’s wort can decrease norethindrone and ethinyl estradiol levels by 13% to 15%, which can result in an unplanned pregnancy.”
Iron supplement interactions
Iron supplements can interact with a few different types of medications.
- Antibiotics and iron: Taking iron alongside certain antibiotics, such as ciprofloxacin, tetracycline, or minocycline, may decrease your body’s absorption of the antibiotic prescription. Check with your healthcare provider before combining antibiotics and iron. They may recommend separating them by a few hours.
- Thyroid hormone and iron: Additionally, those taking synthetic thyroid hormone replacement such as Synthroid (levothyroxine) should be sure to discuss with your healthcare provider all vitamin and mineral supplements that contain iron—also soy, and calcium, which, “if taken within four hours of taking a synthetic thyroid hormone, may reduce the absorption rate,” Dr. Cole says.
Vitamin E and blood thinners
Vitamin E thins the blood. If you’re taking aspirin or a prescription blood thinner (such as warfarin), your risk of internal bleeding is increased, which may even be life-threatening. The same is true of the supplement ginkgo biloba. Consult a healthcare provider before taking any vitamins or supplements with your blood thinner.
Magnesium interactions
Magnesium supplements can disrupt the efficacy of several medications.
- Magnesium and antibiotics: The efficacy of quinolones such as ciprofloxacin—and tetracycline antibiotics such as doxycycline—can be decreased when combined with magnesium supplements. To avoid this interaction, take the antibiotic more than 2 hours before or 6 hours after you take magnesium (or a vitamin or supplement that contains magnesium).
- Magnesium and calcium channel blockers: Taking magnesium along with a calcium channel blocker like nifedipine, amlodipine, diltiazem, felodipine, or verapamil can increase your odds of dizziness and low blood pressure.
- Magnesium and certain diabetes medications: Taking antacids that contain magnesium hydroxide can increase the absorption of the diabetes medications glipizide or glyburide, which can cause low blood sugar. Consult with your provider before combining the two.
- Magnesium and digoxin: If you’ve been prescribed Lanoxin (digoxin), your provider will carefully monitor your digoxin levels. That’s because magnesium can decrease digoxin levels, making digoxin less effective. Talk to your provider if you’re using magnesium supplements or any medications that contain magnesium, so they can adjust your treatment as needed.
- Magnesium and levothyroxine: Antacids or vitamins/supplements that contain magnesium may decrease the efficacy of the thyroid medication levothyroxine, so discuss the risks of this combination with your provider if you are taking this drug. In most cases, the interaction can be avoided by separating when you take each medicine for at least 4 hours.
- Magnesium and osteoporosis drugs: If you’re taking alendronate for osteoporosis, magnesium may reduce its absorption. If you’re combining the two, take magnesium at least 30 minutes after you take alendronate.
Certain drugs can make supplements less effective too. For example, antibiotics such as gentamicin, the antifungal amphotericin B, corticosteroids including prednisone, antacids, and insulin may reduce magnesium levels in the body when combined. Both loop diuretics, such as furosemide, and thiazide diuretics, like hydrochlorothiazide, can also decrease your magnesium levels, so your provider may advise you to supplement with magnesium while taking these drugs.
Vitamin C interactions
Vitamin C can interact with several different types of prescription and over-the-counter medications.
- Vitamin C and barbiturates: Anti-seizure medications such as phenobarbital and vitamin C may interact, making either or both less effective. Check with your healthcare provider.
- Vitamin C and chemotherapy: If you’re receiving chemotherapy, check with your provider before taking vitamin C supplements, as it may impact the effectiveness of your treatment.
- Vitamin C and nitrate medications: Taking nitrate medications can cause tolerance over time, meaning that your body gets used to the drug and it has less of an effect. When combined with the heart medications nitroglycerin, isosorbide dinitrate, or isosorbide mononitrate, vitamin C may impact your body’s tolerance to the drugs, where you possibly do not build up a tolerance.
- Vitamin C and oral contraceptives: If you’re taking estrogen-containing birth control pills or hormone replacement therapy (HRT), supplementing with vitamin C may raise your estrogen levels.
- Vitamin C and antibiotics: Taking vitamin C in conjunction with certain antibiotics, including tetracycline, minocycline, or doxycycline, can increase blood levels of the antibiotic and decrease the effectiveness of vitamin C.
Tetracycline coupons | Minocycline coupons
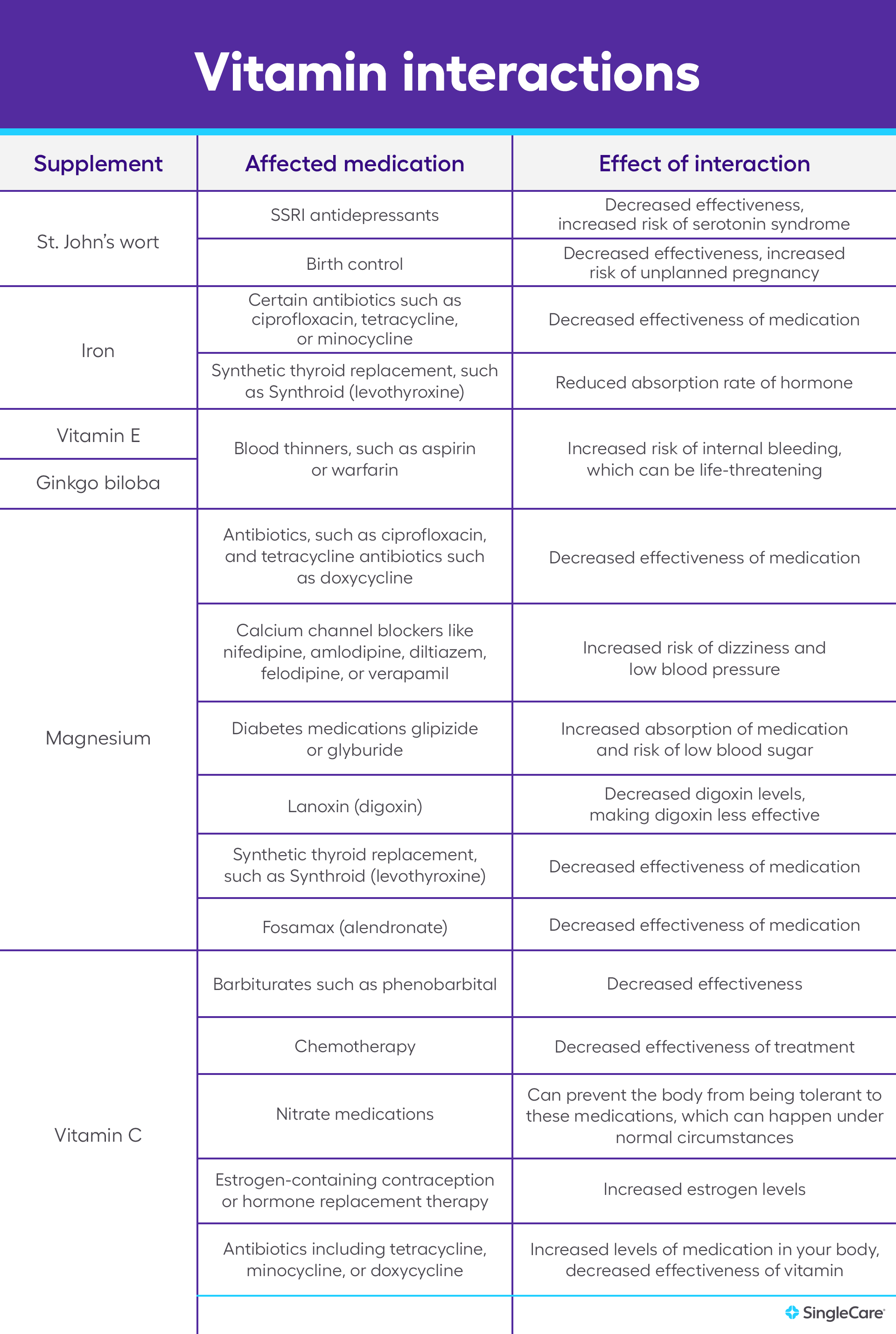
Vitamin interactions chart
8 safety tips for taking supplements and medication
“Prescription medications can deplete nutrients from the body or provide additional nutrients based on the makeup of the medications you’re taking—and that can be helpful or hurtful,” Dr. Cole says. “That’s why it’s important to have an understanding of drug-nutrient interactions if you’re taking both supplements and prescription medications.”
1. Talk to your provider
How certain vitamin interactions occur is largely on a case-by-case basis. Before starting any new vitamins or supplements, be sure to discuss them with your provider. If you’re already taking supplements, it’s important to let your provider know so that they can advise you of any potential interactions and safety concerns. Make a list of all of the supplements you are taking, including the dose and the frequency.
2. Avoid unsafe supplements
To be sure you’re not taking any supplements or herbal remedies that may be dangerous, it’s best to avoid those that claim to treat medical conditions in the same way prescription medicines would. A good rule of thumb is to avoid anything that’s marketed to treat, prevent, or cure diseases.
3. Take as directed
Be sure not to take more of a dietary supplement than recommended. Doing so can increase the risk of serious side effects–for example, fat-soluble vitamins (such as vitamin A, vitamin D, vitamin E, and vitamin K) can accumulate in the body over time, reaching toxic levels. On the other hand, excess water-soluble vitamins are naturally excreted in the urine, so toxicity is rare. It’s also important to take the supplement as directed; for example, with or without food.
4. Space out your doses
Spacing out doses of medications and supplements can help minimize potential interactions and ensure optimal absorption. Consult with your provider for information about potential medication interactions—they may recommend adjusting your medication’s timing so that absorption issues and adverse reactions do not occur.
5. Read labels carefully
Because supplements are held to different standards than prescription and OTC medications–they are not strictly regulated by the FDA–it’s important for consumers to read product labels carefully. A supplement’s label is required to list its active and inactive ingredients as well as the dosage. Before starting the supplement, have a conversation with your healthcare provider. It may also be helpful to research product reviews. Look for supplements that have had third-party testing, such as those that say “USP Verified” or “NSF Certified.”
6. Review supplements before and after surgery
If you are having a surgical procedure, be sure to discuss any vitamins and herbal supplements that you are taking with your doctor beforehand, even common supplements that you may think are harmless. Some supplements may increase the risk of bleeding in patients, and you may be advised to stop them for a period of time before and after surgery.
7. Use extra caution if you’re pregnant or nursing
Pregnant or nursing women should take a prenatal vitamin that contains folic acid. Consult your healthcare provider for guidance on a prenatal vitamin that is right for you. Besides that, if you are pregnant, planning to become pregnant, or breastfeeding, always check with your healthcare provider before starting any new medications, vitamins, or supplements.
It’s also important to consult the pediatrician before giving any supplements to a child because dietary supplements are often not sufficiently tested among these populations.
8. Stay hydrated
Adequate water intake is crucial for overall health. It can also allow your body to metabolize medications and supplements effectively, supporting kidney function for filtering out waste. Dehydration can concentrate substances in your bloodstream, increasing the risk of side effects and interactions. Plus, many supplements require sufficient water for optimal absorption. Drinking enough water throughout the day promotes a safer and more effective experience.
The bottom line
Vitamins and other dietary supplements can offer many health benefits, but they have the potential to interact with prescription medications. Consult your healthcare provider before adding any new supplements to your routine, especially if you’re already on medication. Although a balanced diet is the best source of essential nutrients, there are instances where supplementation may be recommended. A healthcare professional can guide you toward the best options.
- Nearly 40 percent of Americans taking prescription medications and dietary supplements don’t know about drug-nutrient interactions, new survey finds, PR Newswire (2018)
- Are dietary supplements safe?, American Cancer Society (2023)
- The best foods for vitamins and minerals, Harvard Health Publishing (2024)
- Mixing medications and dietary supplements can endanger your health, U.S. Food & Drug Administration (2022)
- Dietary supplements: What you need to know, National Institutes of Health (2023)
- Timing in drug absorption and disposition: The past, present, and future of chronopharmacokinetics, British Journal of Pharmacology (2020)
- Why is third-party certification important for dietary supplements?, Operation Supplement Safety (2024)
- Nursing fundamentals: Chapter 14, nutrition, National Library of Medicine (2021)
- Dietary supplements and bleeding, Baylor University Medical Center Proceedings (2022)
- Interactions between food and drugs, and nutritional status in renal patients: A narrative review, Nutrients (2022)




